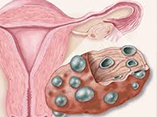
Effect of Trans-Anethole on Gene Expression of Steroidogenic Enzymes in the Ovary of Polycystic Ovary Syndrome Model Rate
DOI:
https://doi.org/10.31661/gmj.v11i.2219Keywords:
Polycystic Ovary Syndrome, Trans-anethole, Cyp17, Aromatase, SteroidogenesisAbstract
Background: The process of steroidogenesis is crucial to the normal function of the ovaries. In individuals with polycystic ovary syndrome (PCOS), the activity of related enzymes in this process is disrupted. In the present study, the effect of trans-anethole was investigated on gene expression of steroidogenesis enzymes in PCOS model rats. Materials and Methods: In this experimental study, thirty female rats were divided into six groups (n=5 per group). Fifteen PCOS rats in three groups received intraperitoneal injections of distilled water, 50, and
80 mg/kg of trans-anethole, respectively. Also, 15 intact rats in three groups received intraperitoneal injections of distilled water, 50, and 80 mg/kg trans-anethole. The expression of steroidogenesis genes was determined using real-time reverse transcription polymerase chain reaction. Results: The mRNA level of Cyp19 significantly increased in intact rats receiving 80 mg/kg trans-anethole compared to the control group. The Cyp19 level in PCOS groups was significantly reduced compared to the control group. The mRNA level of Cyp19 in PCOS groups that resived 50 or 80 mg/kg trans-anethole increased compared to PCOS rats, but this increase was not statistically significant. The mRNA level of Cyp17 did not significantly change in intact and PCOS rats that received trans-anethole compared to the control group. Conclusion: Trans-anethole may improve PCOS complications due to its involvement in regulating steroidogenesis.
References
Yao Q, Shi R, Wang C, Han W, Gao Y, Zhang Y, et al. Cord blood Per- and polyfluoroalkyl substances, placental steroidogenic enzyme, and cord blood reproductive hormone. Environment International. 2019;129:573-82. https://doi.org/10.1016/j.envint.2019.03.047PMid:31174145 Hu Z, Shen W, Kraemer F, Azhar S. Regulation of adrenal and ovarian steroidogenesis by miR-132. J Mol Endocrinol. 2017;59(3):269-83. https://doi.org/10.1530/JME-17-0011PMid:28729436 PMCid:PMC6376965 Saddick S. Identifying genes associated with the development of human polycystic ovary syndrome. Saudi J Biol Sci. 2020;27(5):1271-9. https://doi.org/10.1016/j.sjbs.2020.01.012PMid:32346335 PMCid:PMC7183000 Schiffer L, Barnard L, Baranowski E, Gilligan L, Taylor A, Arlt W, et al. Human steroid biosynthesis, metabolism and excretion are differentially reflected by serum and urine steroid metabolomes: A comprehensive review. J Steroid Biochem Mol Biol. 2019;194:105439. https://doi.org/10.1016/j.jsbmb.2019.105439PMid:31362062 PMCid:PMC6857441 Gareis N, Huber E, Hein G, RodrÃguez F, Salvetti N, Angeli E, et al. Impaired insulin signaling pathways affect ovarian steroidogenesis in cows with COD. Anim Reprod Sci. 2018; 192:298-312. https://doi.org/10.1016/j.anireprosci.2018.03.031PMid:29622349 Bourgneuf C, Bailbé D, Lamazière A, Dupont C, Moldes M, Farabos D, et al. The Goto-Kakizaki rat is a spontaneous prototypical rodent model of polycystic ovary syndrome. Nat Commun. 2021;12(1):1064. https://doi.org/10.1038/s41467-021-21308-yPMid:33594056 PMCid:PMC7886868 Unfer V, Dinicola S, Laganà A, Bizzarri M. Altered Ovarian Inositol Ratios May Account for Pathological Steroidogenesis in PCOS. Int J Mol Sci. 2020;21(19):7157. https://doi.org/10.3390/ijms21197157PMid:32998310 PMCid:PMC7582282 Bakhshalizadeh S, Amidi F, Alleyassin A, Soleimani M, Shirazi R, Shabani Nashtaei M. Modulation of steroidogenesis by vitamin D3 in granulosa cells of the mouse model of polycystic ovarian syndrome. Syst Biol Reprod Med. 2017;63(3):150-61. https://doi.org/10.1080/19396368.2017.1296046PMid:28345956 Song A, Park Y, Kim B, Lee S. Modulation of Lipid Metabolism by Trans-Anethole in Hepatocytes. Molecules. 2020;25(21):4946. https://doi.org/10.3390/molecules25214946PMid:33114589 PMCid:PMC7662808 Samadiâ€Noshahr Z, Hadjzadeh M, Moradiâ€Marjaneh R, Khajaviâ€Rad A. The hepatoprotective effects of fennel seeds extract and trans â€Anethole in streptozotocinâ€induced liver injury in rats. Food Sci Nutr. 2020;9(2):1121-31. https://doi.org/10.1002/fsn3.2090PMid:33598196 PMCid:PMC7866591 Cruz G, Wanderley-Teixeira V, Oliveira J, D' assunção C, Cunha F, Teixeira Ã, et al. Effect of trans-anethole, limonene and your combination in nutritional components and their reflection on reproductive parameters and testicular apoptosis in Spodoptera frugiperda (Lepidoptera: Noctuidae). Chem Biol Interact. 2017;263:74-80. https://doi.org/10.1016/j.cbi.2016.12.013PMid:27989598 Haghighat Gollo Kh, Mahmoudi F, Bayrami A, Zahri S. Influences of L-DOPA and blocking dopamine receptors on aromatase gene expression and serum concentration of LH in polycystic ovary syndrome model rats. Journal of Fasa University of Medical Sciences. 2020;10(3):2448-55. Panghiyangani R, Soeharso P, Andrijono, Suryandari D, Wiweko B, Kurniati M, et al. CYP19A1 gene expression in patients with polycystic ovarian syndrome. J Hum Reprod Sci. 2020;13(2):100-3. https://doi.org/10.4103/jhrs.JHRS_142_18PMid:32792756 PMCid:PMC7394102 Yancu D, Vaillancourt C, Sanderson J. Evaluating the effects on steroidogenesis of estragole and trans-anethole in a feto-placental co-culture model. Mol Cell Endocrinol. 2019;498:110583. https://doi.org/10.1016/j.mce.2019.110583PMid:31536780 Sá N, Ferreira A, Sousa F, Duarte A, Paes V, Cadenas J, et al. First pregnancy after in vitro culture of early antral follicles in goats: Positive effects of anethole on follicle development and steroidogenesis. Mol Reprod Dev. 2020;87(9):966-77. https://doi.org/10.1002/mrd.23410PMid:32761832 Mancini A, Silvestrini A. Oxidative Stress in Metabolic and Endocrine Diseases: Basic and Translational Aspects. Int J Mol Sci. 2022;23(8):4346. https://doi.org/10.3390/ijms23084346PMid:35457165 PMCid:PMC9027438 Ryu S, Seol G, Park H, Choi I. Trans-anethole protects cortical neuronal cells against oxygen-glucose deprivation/reoxygenation. Neurol Sci. 2014;35(10):1541-7. https://doi.org/10.1007/s10072-014-1791-8PMid:24777545 Ajmal N, Khan S, Shaikh R. Polycystic ovary syndrome (PCOS) and genetic predisposition: A review article. Eur J Obstet Gynecol Reprod Biol X. 2019;3:100060. https://doi.org/10.1016/j.eurox.2019.100060PMid:31403134 PMCid:PMC6687436 Pandit K, Kumar A, Kaur S, Kumar V, Jain SK, Bhardwaj R, Kaur S. Amelioration of oxidative stress by trans-Anethole via modulating phase I and phase II enzymes against hepatic damage induced by CCl4 in male Wistar rats. Environ Sci Pollut Res Int. 2022;29(4):6317-33. https://doi.org/10.1007/s11356-021-16070-zPMid:34453252 Al-Omar Z, Ozbakir B, Tulay P. Differential expression of genes involved in steroidogenesis pathway in human oocytes obtained from patients with polycystic ovaries. J Reprod Immunol. 2020;142:103191. https://doi.org/10.1016/j.jri.2020.103191PMid:32937223 Jahromi MS, Tehrani FR, Noroozzadeh M, Zarkesh M, Ghasemi A, Zadeh-Vakili A. Elevated expression of steroidogenesis pathway genes; CYP17, GATA6 and StAR in prenatally androgenized rats. Gene. 2016;593(1):167-71. https://doi.org/10.1016/j.gene.2016.07.067PMid:27511375 Yu KL, Zhang XL, Tan XM, Ji MM, Chen Y, Liu MM, Yu ZL. Distinctive genes involved in steroidogenesis associated with follicular abnormal development in polycystic ovary syndrome model. Reprod Dev Med. 2019;3(3):141-7. https://doi.org/10.4103/2096-2924.268157 Cardoso N, Ribeiro V, Dutra S, Ferriani R, Gastaldi A, Araújo J, et al. Polycystic ovary syndrome associated with increased adiposity interferes with serum levels of TNF-alpha and IL-6 differently from leptin and adiponectin. Arch Endocrinol Metab. 2020;64(1):4-10. https://doi.org/10.20945/2359-3997000000197PMid:32187268 Alissa EM, Algarni SA, Khaffji AJ, Al Mansouri NM. Role of inflammatory markers in polycystic ovaries syndrome: In relation to insulin resistance. Journal of Obstetrics and Gynaecology Research. 2021;47(4):1409-15. https://doi.org/10.1111/jog.14684PMid:33522094 Kim K, Lee H, Seol G. Anti-inflammatory effects of trans -anethole in a mouse model of chronic obstructive pulmonary disease. Biomed Pharmacother. 2017;91:925-30. https://doi.org/10.1016/j.biopha.2017.05.032PMid:28511344 Matboli M, Hasanin AH, Hamady S, Khairy E, Mohamed RH, Aboul-Ela YM, et al. Anti-inflammatory effect of trans-anethol in a rat model of myocardial ischemia-reperfusion injury. Biomed Pharmacother. 2022;150:113070. https://doi.org/10.1016/j.biopha.2022.113070PMid:35658236 Wang W, Zheng J, Cui N, Jiang L, Zhou H, Zhang D, et al. Baicalin ameliorates polycystic ovary syndrome through AMP-activated protein kinase. J Ovarian Res. 2019;12(1):109. https://doi.org/10.1186/s13048-019-0585-2PMid:31722718 PMCid:PMC6852906 González F. Inflammation in Polycystic Ovary Syndrome: Underpinning of insulin resistance and ovarian dysfunction. Steroids. 2012;77(4):300-5. https://doi.org/10.1016/j.steroids.2011.12.003PMid:22178787 PMCid:PMC3309040