Compared Dexmedetomidine and Fentanyl on Sensory-Motor Block in Unilateral Intrathecal Anesthesia of Lower-limbs Orthopedic Surgeries: A Randomized Duble-blind Trials
DOI:
https://doi.org/10.31661/gmj.v11i.2499Keywords:
Unilateral Intrathecal Anesthesia, Sensory-motor Block, Dexmedetomidine, Bupivacaine, FentanylAbstract
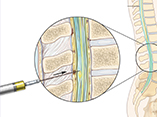
Background: One of the alternatives for lower-limb orthopedic surgery is spinal anesthesia. It can affect the hemodynamic status and cause the prolonged motor and sensory blocks, as well as urinary retention, which are less common in the unilateral technique. Different drugs are used to improve the quality of the block and reduce its complications. Dexmedetomidine, a selective alpha-2 adrenergic receptor agonist, and fentanyl, an opioid medication, could administration as an adjuvant to increase the intrathecal block quality. Hence, this study aimed to compare unilateral spinal anesthesia with bupivacaine/dexmedetomidine (BD) and bupivacaine/fentanyl (BF) regimes on the sensory-motor block among patients with lower-limb orthopedic surgeries. Materials and Method: This randomized, double-blind clinical trial was performed on 36 patients who underwent lower-limb orthopedic surgeries in Qaem Hospital, Mashhad, Iran. The patients were randomly divided into two groups. Patients who received 5.7 mg hyperbaric bupivacaine 0.5% plus 10 µg fentanyl (BF group) or 5 µg dexmedetomidine (BD group) were administered for inducing unilateral spinal anesthesia. Patients and investigators responsible for data collection were not awarded from allocation groups. The sensory-motor block level, duration, postoperative analgesia, and complications were recorded and compared between the two groups. Results: No significant difference was observed between the two groups in hemodynamic changes (i.e., systolic and diastolic blood pressure and heart rate) before and after the blockage (P˃0.05). Also, there was no difference in the sensory-motor block level and anesthesia-related complications between BF and BD groups (P˃0.05). Conclusion: In patients for whom the use of opioids for unilateral spinal anesthesia is contraindicated, dexmedetomidine could be considered an appropriate alternative.
References
Imbelloni LE, Beato L, Cordeiro JA. Unilateral spinal anesthesia with low 0.5% hyperbaric bupivacaine dose. Rev Bras Anestesiol. 2004;54(5):700-6. https://doi.org/10.1590/S0034-70942004000500013PMid:19471781 Kiasari AZ, Babaei A, Alipour A, Motevalli S, Baradari AG. Comparison of hemodynamic changes in unilateral spinal anesthesia versus epidural anesthesia below the T10 sensory level in unilateral surgeries: a double-blind randomized clinical trial. Med Arch. 2017;71(4):274. https://doi.org/10.5455/medarh.2017.71.274-279PMid:28974849 PMCid:PMC5585788 Tekye SM, Alipour M. Comparison of the effects and complications of unilateral spinal anesthesia versus standard spinal anesthesia in lower-limb orthopedic surgery. Braz J Anesthesiol. 2014;64:173-6. https://doi.org/10.1016/j.bjane.2013.06.014PMid:24907876 Liu SS, Ware PD, Allen HW, Neal JM, Pollock JE. Dose-response characteristics of spinal Bupivacaine in volunteers: clinical implications for ambulatory anesthesia. Anesthesiology. 1996;85(4):729-36. https://doi.org/10.1097/00000542-199610000-00007PMid:8873542 Sun S, Wang J, Bao N, Chen Y, Wang J. Comparison of dexmedetomidine and Fentanyl as local anesthetic adjuvants in spinal anesthesia: a systematic review and meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2017;11:3413. https://doi.org/10.2147/DDDT.S146092PMid:29238167 PMCid:PMC5716323 Khan AL, Singh RB, Tripathi RK, Choubey S. A comparative study between intrathecal dexmedetomidine and Fentanyl as adjuvant to intrathecal Bupivacaine in lower abdominal surgeries: A randomized trial. Anesth Essays Res. 2015;9(2):139. https://doi.org/10.4103/0259-1162.156284PMid:26417118 PMCid:PMC4563960 Mahendru V, Tewari A, Katyal S, Grewal A, Singh MR, Katyal R. A comparison of intrathecal dexmedetomidine, clonidine, and Fentanyl as adjuvants to hyperbaric Bupivacaine for lower limb surgery: A double blind controlled study. J Anaesthesiol Clin Pharmacol. 2013;29(4):496. https://doi.org/10.4103/0970-9185.119151PMid:24249987 PMCid:PMC3819844 Li Z, Tian M, Zhang CY, Li AZ, Huang AJ, Shi CX, et al. A randomised controlled trial to evaluate the effectiveness of intrathecal Bupivacaine combined with different adjuvants (Fentanyl, clonidine and dexmedetomidine) in caesarean section. Drug Res. 2015;65(11):581-6. https://doi.org/10.1055/s-0034-1395614PMid:25504002 Shah A, Patel I, Gandhi R. Haemodynamic effects of intrathecal dexmedetomidine added to ropivacaine intraoperatively and for postoperative analgesia. Int J Basic Clin Pharmacol. 2013;2:26-9. https://doi.org/10.5455/2319-2003.ijbcp20130105 Gupta R, Verma R, Bogra J, Kohli M, Raman R, Kushwaha JK. A Comparative study of intrathecal dexmedetomidine and Fentanyl as adjuvants to Bupivacaine. J Anaesthesiol Clin Pharmacol. 2011;27(3):339-43. https://doi.org/10.4103/0970-9185.83678PMid:21897504 PMCid:PMC3161458 Nayagam HA, Singh NR, Singh HS. A prospective randomized double blind study of intrathecal Fentanyl and dexmedetomidine added to low dose bupivacaine for spinal anesthesia for lower abdominal surgeries. Indian J Anaesth. 2014;58(4):430-5. https://doi.org/10.4103/0019-5049.138979PMid:25197111 PMCid:PMC4155288 Basuni AS, Ahmed Ezz HA. Dexmedetomidine as supplement to low-dose levobupivacaine spinal anesthesia for knee arthroscopy. Egypt J Anaesth. 2014;30(2):149-53. https://doi.org/10.1016/j.egja.2013.11.003 Taher-Baneh N, Ghadamie N, Sarshivi F, Sahraie R, Nasseri K. Comparação de fentanil e dexmedetomidina como adjuvante à bupivacaÃna para raquianestesia unilateral em cirurgia de membros inferiores: estudo randômico. Braz J Anesthesiol. 2019;69(4):369-76. https://doi.org/10.1016/j.bjan.2019.03.005PMid:31362883 PMCid:PMC9391866