Relationship Between Personality Traits and Perceived Pain After Photorefractive Keratectomy: A Cross-Sectional Study in Hamadan
Personality Traits and Perceived Pain After PRK
DOI:
https://doi.org/10.31661/gmj.v13i.2989Abstract
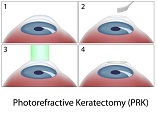
Background: Photorefractive keratectomy (PRK) is a common procedure to correct refractive errors. However, postoperative pain is one of the most common drawbacks of PRK. Evidence shows that individual`s personality traits could impact postoperative perceived pain. Hence, this study aimed to investigate the severity of postoperative pain and personality traits after PRK.
Materials and Methods: This cross-sectional study was performed on 300 patients who attended to Mahdieh Surgical Clinic (Hamadan, Iran) and underwent PRK. Persian version of the NEO Five-Factor Inventory (NEO-FFI) was applied to assess personality traits, and postoperative pain was measured using the visual analog scale (VAS) score.
Results: The mean age of patients was 31.8 ±5.51 years, and most (68%) were female. The most common personality trait was neuroticism, and the mean refractive errors of the right and left eyes of the patients were 1.2±2.67 and 1.3±2.75, respectively. Regarding the VAS score, patients with neuroticism traits perceived the most severe postoperative pain (VAS=6±2.2). Also, the Pearson correlation test indicated a positive correlation between perceived pain and neuroticism personality traits (r=0.059, P˂0.001). In contrast, a significant negative correlation was observed between extraversion and conscientiousness with pain perception (r= -0.737 and r= -0.307, respectively).
Conclusion: Our findings showed a positive and significant correlation between three personality traits and pain perception in these patients. Postoperative pain perception in patients undergoing PRK depends on the personality traits of these patients. Groups with less personality stability feel more pain than groups with stable personalities.
References
Vestergaard AH, Hjortdal J, Ivarsen A, Work K, Grauslund J, Sjølie AK. Long-term outcomes of photorefractive keratectomy for low to high myopia: 13 to 19 years of follow-up. J Refract Surg. 2013;29(5):312-9.
https://doi.org/10.3928/1081597X-20130415-02
PMid:23659229
Spadea L, Verboschi F, De Rosa V, Salomone M, Vingolo EM. Long-term results of no-alcohol laser epithelial keratomileusis and photorefractive keratectomy for myopia. Int J Ophthalmol. 2015;8(3):574-9.
Moisseiev E, Sela T, Minkev L. Increased preferences of surface ablation over LASIK between 2008-2011 is correlated to risk of ectasia. Clin Ophthalmol. 2013;7:93-8.
https://doi.org/10.2147/OPTH.S38959
PMid:23345963 PMCid:PMC3548437
Guedj M, Saad A, Audureau E. PRK in patients with suspected KCN; five years follow up. J Cataract Refract Surg. 2013;39(1):66-73.
https://doi.org/10.1016/j.jcrs.2012.08.058
PMid:23102727
Garcia R, Campello Horovitz R, Torricelli A . Improved Evaluation of postoperative Pain after PRK. Cornea. 2016; 35: 205-9.
https://doi.org/10.1097/ICO.0000000000000704
PMid:26655482
Ishihara M, Arai T, Sato S, Morimoto Y, Obara M, Kikuchi M. Temperature measurement for energy-efficient ablation by thermal radiation with a microsecond time constant from the corneal surface during ArF excimer laser ablation. Front Med Biol Eng. 2001;11(3):167-75.
https://doi.org/10.1163/15685570152772441
PMid:11898899
Maldonado-Codina C, Morgan PB, Efron N. Thermal consequences of photorefractive keratectomy. Cornea. 2001;20(5):509-15.
https://doi.org/10.1097/00003226-200107000-00014
PMid:11413408
Shimizutani M, Odagiri Y, Ohya Y, Shimomitsu T, Kristensen TS, Maruta T, et al. Relationship of nurse burnout with personality characteristics and coping behaviors. Ind Health. 2008;46(4):326-35.
https://doi.org/10.2486/indhealth.46.326
PMid:18716380
Treede RD. The International Association for the Study of Pain definition of pain: as valid in 2018 as in 1979, but in need of regularly updated footnotes. Pain Rep. 2018;3(2):e643.
https://doi.org/10.1097/PR9.0000000000000643
PMid:29756089 PMCid:PMC5902252
Hofbauer RK, Rainville P, Duncan GH, Bushnell MC. Cortical representation of the sensory dimension of pain. J Neurophysiol. 2001;86(1):402-11.
https://doi.org/10.1152/jn.2001.86.1.402
PMid:11431520
Rainville P, Feine JS, Bushnell MC, Duncan GH. A psychophysical comparison of sensory and affective responses to four modalities of experimental pain. Somatosens Mot Res. 1992;9(4):265-77.
https://doi.org/10.3109/08990229209144776
PMid:1492527
Esmaeilou Y, Tamaddonfard E, Erfanparast A, Soltanalinejad-Taghiabad F. Behavioral and receptor expression studies on the primary somatosensory cortex and anterior cingulate cortex oxytocin involvement in modulation of sensory and affective dimensions of neuropathic pain induced by partial sciatic nerve ligation in rats. Physiol Behav. 2022;251:113818.
https://doi.org/10.1016/j.physbeh.2022.113818
PMid:35443199
Kim S, Dowgwillo EA, Kratz AL. Examining the Dynamic Relationship between Positive and Negative Emotions as a Function of Pain, Fatigue, and Stress in Individuals with and without Fibromyalgia. The Journal of Pain. 2022;23(5):56-7.
https://doi.org/10.1016/j.jpain.2022.03.213
Feldman SI, Downey G, Schaffer-Neitz R. Pain, negative mood, and perceived support in chronic pain patients: a daily diary study of people with reflex sympathetic dystrophy syndrome. J Consult Clin Psychol. 1999;67(5):776-85.
https://doi.org/10.1037/0022-006X.67.5.776
PMid:10535244
Grouper H, Eisenberg E, Pud D. More insight on the role of personality traits and sensitivity to experimental pain. J Pain Res. 2021;14:1837-44.
https://doi.org/10.2147/JPR.S309729
PMid:34168491 PMCid:PMC8216734
Vassend O, Røysamb E, Nielsen CS. Five-factor personality traits and pain sensitivity: a twin study. Pain. 2013;154(5):722-8.
https://doi.org/10.1016/j.pain.2013.01.010
PMid:23473786
Banozic A, Miljkovic A, Bras M, Puljak L, Kolcic I, Hayward C, et al. Neuroticism and pain catastrophizing aggravate response to pain in healthy adults: an experimental study. Korean J Pain. 2018;31(1):16-26.
https://doi.org/10.3344/kjp.2018.31.1.16
PMid:29372022 PMCid:PMC5780211
Woreta FA, Gupta A, Hochstetler B, Bower KS. Management of post-photorefractive keratectomy pain. Surv Ophthalmol. 2013;58(6):529-35.
https://doi.org/10.1016/j.survophthal.2012.11.004
PMid:24160728
Gadde AK, Srirampur A, Katta KR, Mansoori T, Armah SM. Comparison of single-step transepithelial photorefractive keratectomy and conventional photorefractive keratectomy in low to high myopic eyes. Indian J Ophthalmol. 2020;68(5):755-61.
https://doi.org/10.4103/ijo.IJO_1126_19
PMid:32317441 PMCid:PMC7350485
Anisi J. Validity and reliability of NEO Five-Factor Inventory (NEO-FFI) on university students. International Journal of Behavioral Sciences. 2012;5(4):351-5.
Mohebbi M, Rafat-Nejad A, Mohammadi SF, Asna-Ashari K, Kasiri M, Heidari-Keshel S, et al. Post-photorefractive keratectomy pain and corneal sub-basal nerve density. J Ophthalmic Vis Res. 2017;12(2):151-5.
Mohammadpour M, Khorrami-Nejad M, Shakoor D. Role of artificial tears with and without hyaluronic acid in controlling ocular discomfort following PRK: a randomized clinical trial. Int J Ophthalmol. 2021;14(8):1225-30.
https://doi.org/10.18240/ijo.2021.08.14
PMid:34414088 PMCid:PMC8342296
Baksh BS, Morkin M, Felix E, Karp CL, Galor A. Ocular pain symptoms in individuals with and without a history of refractive surgery: results from a cross-sectional survey. Cornea. 2022;41(1):31-8.
https://doi.org/10.1097/ICO.0000000000002675
PMid:33560674 PMCid:PMC8349379
Palochak CM, Santamaria J, Justin GA, Apsey DA, Caldwell MC, Steigleman WA, et al. Assessment of factors associated with postoperative pain after photorefractive keratectomy. Cornea. 2020;39(10):1215-20.
https://doi.org/10.1097/ICO.0000000000002402
PMid:32558728
Zarei-Ghanavati S, Nosrat N, Morovatdar N, Abrishami M, Eghbali P. Efficacy of corneal cooling on postoperative pain management after photorefractive keratectomy: A contralateral eye randomized clinical trial. J Curr Ophthalmol. 2017;29(4):264-9.
https://doi.org/10.1016/j.joco.2017.04.004
PMid:29270472 PMCid:PMC5735231
Moradi-Farsani D, Naghibi K, Taheri S, Ali-Kiaii B, Rahimi-Varposhti M. Effects of Age and Gender on Acute Postoperative Pain after Cataract Surgery under Topical Anesthesia and Sedation. J Isfahan Med Sch. 2017;34(414):1627-33.
Kadu A, Chopra SS, Gupta N, Jayan B, Kochar GD. Effect of the personality traits of the patient on pain perception and attitude toward orthodontic treatment. J Indian Orthod Soc. 2015;49(2):89-95.
https://doi.org/10.4103/0301-5742.162260
Abu Alhaija ES, AlDaikki A, Al-Omairi MK, Al-Khateeb SN. The relationship between personality traits, pain perception and attitude toward orthodontic treatment. Angle Orthod. 2010;80(6):1141-9.
https://doi.org/10.2319/012710-59.1
PMid:20677967 PMCid:PMC8929492
Tananuvat N, Tansanguan S, Wongpakaran N, Wongpakaran T. Role of neuroticism and perceived stress on quality of life among patients with dry eye disease. Sci Rep. 2022;12(1):7079.
https://doi.org/10.1038/s41598-022-11271-z
PMid:35490178 PMCid:PMC9056508
Hanney WJ, Wilson AT, Smith T, Shiley C, Howe J, Kolber MJ. Personality Type and Chronic Pain: The Relationship between Personality Profile and Chronic Low Back Pain Using Eysenck's Personality Inventory. NeuroSci. 2022;3(4):677-86.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







