Prevalence of Echocardiographic Profile and Its ‘Related Risk Factors in Congenital Heart Disease Patients; A Cross-Sectional Study
Prevalence of Echocardiographic Profile of Congenital Heart Disease Patients
DOI:
https://doi.org/10.31661/gmj.v13i.3517Keywords:
Keywords: Congenital heart disease, Echocardiography, Epidemiology, PediatricsAbstract
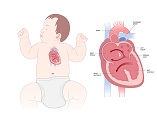
Background: Congenital heart disease (CHD) represents the most common and lethal birth defect affecting newborns. This study aimed to characterize the echocardiographic profile of CHDs, along with their prevalence and associated risk factors in CHD patients. Materials and Methods: This cross‐sectional, analytical study was conducted on CHD patients referred to the major pediatric hospital affiliated with Urmia University of Medical Sciences between March 2022 and October 2023. They were selected by convenience sampling method. The collected data, including mothers' parity, prior diagnoses of heart disease, hypertension, diabetes, thyroid disorders, COVID-19 infection during pregnancy, prior surgical procedures, use of complementary medicine during gestation, medication history, and mode of delivery. Additionally, child-related characteristics were investigated, including age, gender, co-existing congenital cardiovascular disease, neonatal intensive care unit (NICU) admission history, and echocardiographic findings. Specifically, the study focused on abnormalities in left ventricular fractional shortening (LVFS) and left ventricular ejection fraction (LVEF). Data analysis was done using SPSS software version 22.0. Results: Of 293 CHD children, 59.72% were male and 40.27% were female. Overall, 132 (45%) children were below one year of age. Among echocardiography profile, Patent Foramen Ovale (PFO) constituted 65 cases accounting for 22.1% of all CHD cases and Atrial septal defect (ASD) was the second most common CHD accounting for 16.3% of all CHD cases. Mother's infection with Covid-19 during pregnancy (P<0.001), type of delivery (P=0.015), and patient's NICU hospitalization (P=0.010) was statistically significant among the patients with normal and abnormal echocardiography. Conclusion: This study reveals a significant prevalence of Patent Foramen Ovale (PFO) and Atrial Septal Defect (ASD) among patients with congenital heart disease (CHD), highlighting the crucial role of early echocardiographic screening in this group. It also suggests a potential link between maternal COVID-19 infection during pregnancy, the method of delivery, and abnormal echocardiographic findings in CHD patients.
References
Parvar SY, Ghaderpanah R, Naghshzan A. Prevalence of congenital heart disease according to the echocardiography findings in 8145 neonates, multicenter study in southern Iran. Health Sci Rep. 2023; 6(4):e1178.
https://doi.org/10.1002/hsr2.1178
PMid:37033389 PMCid:PMC10073012
van der Linde D, Konings EEM, Slager MA, et al. Birth prevalence of congenital heart disease worldwide. JACC. 2011;58(21):2241‐2247.
https://doi.org/10.1016/j.jacc.2011.08.025
PMid:22078432
Keates AK, Mocumbi AO, Ntsekhe M, Sliwa K, Stewart S. Cardiovascular disease in Africa: epidemiological profile and challenges. Nature Reviews Cardiology. 2017 May;14(5):273-93.
https://doi.org/10.1038/nrcardio.2017.19
PMid:28230175
Liu Y, Chen S, Zühlke L, Black GC, Choy M-K, Li N, et al. Global birth prevalence of congenital heart defects 1970-2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. 2019; 48:455-63.
https://doi.org/10.1093/ije/dyz009
PMid:30783674 PMCid:PMC6469300
Starnes J, Graves J, Aliyu M, Soslow J. RACIAL AND ETHNIC INEQUITIES IN INFANT MORTALITY FROM CONGENITAL HEART DISEASE. Journal of the American College of Cardiology. 2024;83(13_Supplement):1630-.
https://doi.org/10.1016/S0735-1097(24)03620-9
Tulloh RM, Medrano-Lopez C, Checchia PA, Stapper C, Sumitomo N, Gorenflo M, Bae EJ, Juanico A, Gil-Jaurena JM, Wu MH, Farha T. CHD and respiratory syncytial virus: global expert exchange recommendations. Cardiology in the Young. 2017;27(8):1504-21.
https://doi.org/10.1017/S1047951117000609
PMid:28619123
Di Filippo S. Antibioprophylaxie de l'endocardite infectieuse dans les cardiopathies congénitales [Infective endocarditis prophylaxis in congenital heart disease]. Presse Med. 2017;46(6 Pt 1):606-611.
https://doi.org/10.1016/j.lpm.2017.05.016
PMid:28576635
Demelash Enyew H, Bogale BG, Hailu AB, Mereta ST. Environmental exposures and adverse pregnancy outcomes in Ethiopia: A systematic review and meta-analysis. PLoS One. 2023;18(7):e0288240.
https://doi.org/10.1371/journal.pone.0288240
PMid:37437038 PMCid:PMC10337917
Bedair R, Iriart X. EDUCATIONAL SERIES IN CONGENITAL HEART DISEASE: Tetralogy of Fallot: diagnosis to long-term follow-up. Echo Res Pract. 2019;6(1):R9-R23.
https://doi.org/10.1530/ERP-18-0049
PMid:30557849 PMCid:PMC6301192
Ismail SR, Almazmi MM, Khokhar R, AlMadani W, Hadadi A, Hijazi O, Kabbani MS, Shaath G, Elbarbary M. Effects of protocol-based management on the post-operative outcome after systemic to pulmonary shunt. Egypt Heart J. 2018;70(4):271-278.
https://doi.org/10.1016/j.ehj.2018.09.007
PMid:30591742 PMCid:PMC6303540
Albus C, Waller C, Fritzsche K, Gunold H, Haass M, Hamann B, Kindermann I, Koellner V, Leithaeuser B, Marx N, Meesmann M. Significance of psychosocial factors in cardiology: update 2018: Position paper of the German Cardiac Society. Clinical Research in Cardiology. 2019;108:1175-96.
https://doi.org/10.1007/s00392-019-01488-w
PMid:31076853
Hussain MA, Tahura S, Sayeed MA, Rahman MM, Rahman MM, Kar SK. Past and present pattern of congenital heart disease at Dhaka Shishu Hospital: a situation analysis. Bangladesh J Child Health. 2010;34(2):51-.
https://doi.org/10.3329/bjch.v34i2.10217
Pinto Júnior VC, Branco KMPC, Cavalcante RC, et al. Epidemiology of congenital heart disease in Brazil. Revista Brasileira de Cirurgia Cardiovascular. 2015; 30(2):219‐224.
Siabani S. Epidemiology of congenital heart defects in Iran: a systematic review. Online J Cardiol Res Rep. 2019; 2(3):1‐5.
https://doi.org/10.33552/OJCR.2019.02.000537
Lardhi AA. Prevalence and clinical significance of heart murmurs detected in routine neonatal examination. J Saudi Heart Assoc. 2010;22(1):25-7.
https://doi.org/10.1016/j.jsha.2010.03.005
PMid:23960589 PMCid:PMC3727508
Ahmadi A, Gharipour M, Navabi ZS, Heydari H. Risk factors of congenital heart diseases: A hospital‐based case‐control study in Isfahan, Iran. ARYA Atheroscler. 2020;16(1):1‐6.
Pugnaloni F, Felici A, Corno AF, Marino B, Versacci P, Putotto C. Gender differences in congenital heart defects: a narrative review. Transl Pediatr. 2023;12(9):1753-1764.
https://doi.org/10.21037/tp-23-260
PMid:37814719 PMCid:PMC10560357
El-Gilany AH, Yahia S, Wahba Y. Prevalence of congenital heart diseases in children with Down syndrome in Mansoura, Egypt: a retrospective descriptive study. Ann Saudi Med. 2017;37(5):386-392.
https://doi.org/10.5144/0256-4947.2017.386
PMid:28988253 PMCid:PMC6074196
Parvar SY, Ghaderpanah R, Naghshzan A. Prevalence of congenital heart disease according to the echocardiography findings in 8145 neonates, multicenter study in southern Iran. Health Science Reports. 2023;6(4): e1178.
https://doi.org/10.1002/hsr2.1178
PMid:37033389 PMCid:PMC10073012
Cao Y, Huang R, Kong R, Li H, Zhang H, Li Y, Liang L, Xiong D, Han S, Zhou L, Guo J. Prevalence and risk factors for congenital heart defects among children in the Multi-Ethnic Yunnan Region of China. Translational Pediatrics. 2022;11(6):813.
https://doi.org/10.21037/tp-21-371
PMid:35800272 PMCid:PMC9253957
Wu W, He J, Shao X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990‐2017. Medicine. 2020; 99(23): e20593.
https://doi.org/10.1097/MD.0000000000020593
PMid:32502030 PMCid:PMC7306355
Andishmand A, Moghimi S, Namayandeh S, et al. The epidemiological aspects of congenital heart disease in central and southern district of Iran. Adv Biomed Res. 2014; 3:233.
https://doi.org/10.4103/2277-9175.145732
PMid:25538919 PMCid:PMC4260289
Ishikawa T, Iwashima S, Ohishi A, Nakagawa Y, Ohzeki T. Prevalence of congenital heart disease assessed by echocardiography in 2067 consecutive newborns. Acta Paediatr (Stockholm). 2011;100(8): e55‐e60.
https://doi.org/10.1111/j.1651-2227.2011.02248.x
PMid:21362039
Mohsenzadeh a, saket s, Ahmadipour s, Baharvand b. prevalence and types of congenital heart disease in babies born in the city of Khorramabad (2007‐2011). scientific magazine yafte. 2014;15(5):23‐29.
Kafian Atary S, Mirshahi A, Amouzeshi A, et al. Epidemiologic study of congenital heart diseases and its related factors in children referred to the pediatric cardiac clinic of Birjand University of Medical Sciences, Iran. Int J Pediatr. 2019;7(12):10455‐10463.
Mesa D, Franco M, de Lezo JS, Munoz J, Rus C, Delgado M, Ruiz M, Pan M, Romo E, Valles F, Viñals M. Prevalence of patent foramen ovale in young patients with cryptogenic stroke. REVISTA ESPANOLA DE CARDIOLOGIA. 2003 Jul 1;56(7):662-8.
https://doi.org/10.1157/13049647
PMid:12855148
Wiktor DM, Carroll JD. ASD closure in structural heart disease. Current Cardiology Reports. 2018 Jun;20:1-6.
https://doi.org/10.1007/s11886-018-0983-x
PMid:29666940
Rao P.S., Harris A.D. Recent advances in managing septal defects: Atrial septal defects. F1000 Res. 2017;6:2042.
https://doi.org/10.12688/f1000research.11844.1
PMid:29250321 PMCid:PMC5701442
Islam MN, Hossain MA, Khaleque MA, Das MK, Khan MR, Bari MS, Bhuiyan MK. Prevalence of congenital heart disease in neonate in a tertiary level hospital. Nepal Journal of Medical sciences. 2013 Oct 14;2(2):91-5.
https://doi.org/10.3126/njms.v2i2.8942
Rahim F, Ebadi A, Saki G, Remazani A. Prevalence of congenital heart disease in Iran: a clinical study. J Med Sci. 2008;8:547‐552.
https://doi.org/10.3923/jms.2008.547.552
Kishore S, Kumar M, Kumar A, Gupta A, Chandan C, Anshuman A, et al. Clinical and Echocardiographic Profile of Congenital Heart Diseases in the 0-12-Year Age Group in a Tertiary Care Medical Institute in Eastern India: A Retrospective, Cross-Sectional Study. Cureus. 2022 Jun;14(6):e26114.
https://doi.org/10.7759/cureus.26114
Chakraborty A, Gorla SR, Swaminathan S. Impact of prenatal diagnosis of complex congenital heart disease on neonatal and infant morbidity and mortality. Prenatal diagnosis. 2018 Nov;38(12):958-63.
https://doi.org/10.1002/pd.5351
PMid:30171818
do Amaral Lopes SA, Guimarães IC, Costa SF, Acosta AX, Abe-Sandes K, Mendes CM. Risk factors for critical and complex congenital heart diseases: Case-control study. Progress in Pediatric Cardiology. 2023 Mar 1;68:101612.
https://doi.org/10.1016/j.ppedcard.2022.101612
Ornoy A, Becker M, Weinstein-Fudim L, Ergaz Z. Diabetes during Pregnancy: A Maternal Disease Complicating the Course of Pregnancy with Long-Term Deleterious Effects on the Offspring A Clinical Review. In J Mol Sci. 2021 Mar;22(6):2965.
https://doi.org/10.3390/ijms22062965
PMid:33803995 PMCid:PMC7999044
Yang J, Qiu H, Qu P, Zhang R, Zeng L, Yan H. Prenatal Alcohol Exposure and Congenital Heart Defects: A Meta-Analysis. PLoS One. 2015 Jun 25;10(6):e0130681.
https://doi.org/10.1371/journal.pone.0130681
PMid:26110619 PMCid:PMC4482023
Al-Biltagi M, El Razaky O, El Amrousy D. Cardiac changes in infants of diabetic mothers. World J Diabetes. 2021 Aug 15;12(8):1233-1247.
https://doi.org/10.4239/wjd.v12.i8.1233
PMid:34512889 PMCid:PMC8394229
Arendt LH, Pedersen LH, Pedersen L, Ovesen PG, Henriksen TB, Lindhard MS, Olsen J, Sørensen HT, Ramlau-Hansen CH. Glycemic control in pregnancies complicated by pre-existing diabetes mellitus and congenital malformations: a Danish population-based study. Clinical epidemiology. 2021 Jul 26:615-26.
https://doi.org/10.2147/CLEP.S298748
PMid:34345185 PMCid:PMC8325058
Salavaty Zadeh M, Kumar Mandal S. Herbal Remedies for Pediatric Earache in Traditional Iranian Medicine. Plant Biotechnology Persa. 2024; 6 (1): 65-68.
https://doi.org/10.61186/pbp.6.1.65
Ahmadi M, Khajoei Nejad F, Dastyar N. Identification of important herbs for anti-fever treatment: an ethnobotanical study of Sojas Rud, northwest Iran. Journal of Biochemicals and Phytomedicine. 2023; 2(2): 54-58.
https://doi.org/10.34172/jbp.2023.11
Zolfigol A, Pirhadi M. Phytotherapy in Children's Colic. Plant Biotechnology Persa. 2024; 6 (2): 89-94.
Ganguly P, Mandal SK, Mondal P, Sen DJ. Medicinal plants effective against dengue fever in India: A brief review. Journal of Biochemicals and Phytomedicine. 2024; 3(1): 14-17.
Saki F, Basiratnia M. Congenital Limb Anomaly as a New Presentation of Arthrogryposis-Renal Problems-Cholestasis (ARC) Syndrome in an Iranian Infant: A Case Report. Galen Medical Journal. 2015 Aug 4;4(3): e285-.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







