Biological and Synthetic Materials in Mandibular Reconstruction
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3533Keywords:
Mandibular Reconstruction; Biological Materials; Synthetic Materials; Autografts; Allografts; Xenografts; Titanium; Polymeric Materials; Ceramic Materials; Bone RegenerationAbstract
Mandibular reconstruction is a critical surgical procedure necessary for restoring both function and aesthetics following trauma, tumor resection, or congenital defects. Over time, a variety of biological and synthetic materials have been developed to address the challenges of reconstructing the complex anatomy of the mandible. Biological materials, such as autografts, offer superior biocompatibility and osteogenic potential, but are limited by donor site morbidity and graft availability. Allografts and xenografts provide more accessible alternatives but are associated with higher risks of immune rejection and slower integration. In contrast, synthetic materials like titanium, PEEK (polyether ether ketone), and hydroxyapatite provide excellent mechanical strength and durability but often lack osteoinductive properties, requiring surface modifications to improve tissue integration.
This review aims to provide a comprehensive analysis of the current materials used in mandibular reconstruction, comparing their biocompatibility, mechanical properties, osteoinductive potential, and clinical outcomes. Additionally, the review explores the growing role of composite materials that combine the strength of synthetics with the biological activity of natural tissues, as well as the advent of tissue engineering approaches that incorporate stem cell therapies and biomaterial scaffolds to promote bone regeneration. Emerging technologies such as 3D printing of custom-made implants and the application of nanotechnology for enhanced integration and infection control are also discussed as promising directions for future clinical applications. The findings highlight the need for continued research into optimizing biomaterial design and improving regenerative therapies to enhance patient-specific outcomes, reduce complications, and foster successful long-term integration of reconstructed mandibular structures. This review provides a roadmap for advancing both material science and clinical practice in the field of mandibular reconstruction.
References
Goh B, Lee S, Tideman H, Stoelinga P. Mandibular reconstruction in adults: a review. International journal of oral and maxillofacial surgery. 2008;37 7:597-605.
https://doi.org/10.1016/j.ijom.2008.03.002
PMid:18450424
Mehta R, Deschler D. Mandibular reconstruction in 2004: an analysis of different techniques. Current Opinion in Otolaryngology & Head and Neck Surgery. 2004;12:288-93.
https://doi.org/10.1097/01.moo.0000131444.50445.9d
PMid:15252248
Morrison A, Brady J. Mandibular reconstruction using nonvascularized autogenous bone grafting. Current Opinion in Otolaryngology & Head and Neck Surgery. 2010 Aug 1;18(4):227-31.
https://doi.org/10.1097/MOO.0b013e32833a46ed
PMid:20508523
Baldwin PC, Li DJ, Auston D, Mir H, Yoon R, Koval K. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. Journal of Orthopaedic Trauma. 2019;33:203-13.
https://doi.org/10.1097/BOT.0000000000001420
PMid:30633080
Correia F, Pozza D, Gouveia S, Felino A, Faria-Almeida R. Advantages of Porcine Xenograft over Autograft in Sinus Lift: A Randomised Clinical Trial. Materials. 2021;14(12):3439.
https://doi.org/10.3390/ma14123439
PMid:34205826 PMCid:PMC8234120
Kannan R, Wei G, Ma PX. Synthetic polymeric biomaterials for tissue engineering In: Tissue Engineering Using Ceramics and Polymers . Elsevier. 2022; 2024: 41-74.
https://doi.org/10.1016/B978-0-12-820508-2.00023-4
PMid:35966405 PMCid:PMC9373874
Wang L, Su Y xiong, Zheng G, Liao G, Zhang W. Healing masseter entheses of mandibular reconstruction with autograft-Raman spectroscopic and histological study. International journal of oral and maxillofacial surgery. 2013;42 7:915-22.
https://doi.org/10.1016/j.ijom.2012.12.010
PMid:23369657
Giedraitis A, Arnoczky SP, Bedi A. Allografts in Soft Tissue Reconstructive Procedures: Important Considerations. Sports Health: A Multidisciplinary Approach. 2014 May;6(3):256-64.
https://doi.org/10.1177/1941738113503442
PMid:24790696 PMCid:PMC4000469
Fishman JA, Mueller NJ. Infectious Diseases and Clinical Xenotransplantation. Emerg Infect Dis. 2024 Jul;30(7):1311-8.
https://doi.org/10.3201/eid3007.240273
PMid:38916550 PMCid:PMC11210669
Lin L, Wang H, Ni M, Rui Y, Cheng TY, Cheng CK, et al. Enhanced osteointegration of medical titanium implant with surface modifications in micro/nanoscale structures. Journal of Orthopaedic Translation. 2014 Jan;2(1):35-42.
https://doi.org/10.1016/j.jot.2013.08.001
García-Gareta E, Coathup MJ, Blunn GW. Osteoinduction of bone grafting materials for bone repair and regeneration. Bone. 2015 Dec;81:112-21.
https://doi.org/10.1016/j.bone.2015.07.007
PMid:26163110
Moura LB, Carvalho PHDA, Xavier CB, Post LK, Torriani MA, Santagata M, et al. Autogenous non-vascularized bone graft in segmental mandibular reconstruction: a systematic review. International Journal of Oral and Maxillofacial Surgery. 2016 Nov;45(11):1388-94.
https://doi.org/10.1016/j.ijom.2016.05.004
PMid:27237079
Ma H, Dessel JV, Shujaat S, Bila M, Gu Y, Sun Y, et al. Long-term functional outcomes of vascularized fibular and iliac flap for mandibular reconstruction: A systematic review and meta-analysis. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2020; 74(2):247-58.
https://doi.org/10.1016/j.bjps.2020.10.094
PMid:33277215
Sudhakar K, Mohanty R, Singh V. Evaluation of Donor Site Morbidity Associated with Iliac Crest Bone Harvest in Oral and Maxillofacial, Reconstructive Surgery. Journal of clinical and diagnostic research : JCDR. 2017;11 6:ZC28-33.
https://doi.org/10.7860/JCDR/2017/28688.10053
PMid:28764289 PMCid:PMC5535479
Ferretti C, Muthray E, Rikhotso E, Reyneke J, Ripamonti U. Reconstruction of 56 mandibular defects with autologous compressed particulate corticocancellous bone grafts. The British journal of oral & maxillofacial surgery. 2016;54 3:322-6.
https://doi.org/10.1016/j.bjoms.2015.12.014
PMid:26805463
Katz MS, Ooms M, Heitzer M, Peters F, Winnand P, Kniha K, et al. Postoperative Morbidity and Complications in Elderly Patients after Harvesting of Iliac Crest Bone Grafts. Medicina. 2021 Jul 27;57(8):759.
https://doi.org/10.3390/medicina57080759
PMid:34440965 PMCid:PMC8401410
Kessler P, Thorwarth M, Bloch-Birkholz A, Nkenke E, Neukam FW. Harvesting of bone from the iliac crest-comparison of the anterior and posterior sites. British Journal of Oral and Maxillofacial Surgery. 2005 Feb;43(1):51-6.
https://doi.org/10.1016/j.bjoms.2004.08.026
PMid:15620775
Palmer WJ, Nelms L. Face transplantation for massive mandibular defects: considerations for allograft design and surgical planning. Plastic and Aesthetic Research. 2020;7:2.
https://doi.org/10.20517/2347-9264.2019.34
Han G, Wang Y, Bi W, Jia J, Wang W, Xu M, et al. Reconstruction using massive allografts after resection of extremity osteosarcomas the study design: A retrospective cohort study. International Journal of Surgery. 2015 Sep;21:108-11.
https://doi.org/10.1016/j.ijsu.2015.07.686
PMid:26232712
Delloye C, van Cauter M, Dufrane D, Francq BG, Docquier PL, Cornu O. Local complications of massive bone allografts: an appraisal of their prevalence in 128 patients. Acta Orthop Belg. 2014 Jun;80(2):196-204.
Bus MPA, Dijkstra PDS, Van De Sande MAJ, Taminiau AHM, Schreuder HWB, Jutte PC, et al. Intercalary Allograft Reconstructions Following Resection of Primary Bone Tumors: A Nationwide Multicenter Study. Journal of Bone and Joint Surgery. 2014 Feb 19;96(4):e26.
https://doi.org/10.2106/JBJS.M.00655
PMid:24553895
Carvalho PH de A, Trento G dos S, Moura L, Cunha G, Gabrielli MA, Pereira-Filho V. Horizontal ridge augmentation using xenogenous bone graft-systematic review. Oral and Maxillofacial Surgery. 2019;23:271-9.
https://doi.org/10.1007/s10006-019-00777-y
PMid:31089897
Agop-Forna D, Törok R, Törok B, Dragomir R, Ehrenfest DMD, Dascălu C, et al. Postoperative Study of Bone Gain in Mandibular Alveolar Bone Reconstructed with Screw-Guided Bone Regeneration Technique and Porcine-Derived Xenograft in 42 Edentulous Patient Candidates for Implant-Prosthetic Therapy. Applied Sciences. 2021;11(21):9826.
https://doi.org/10.3390/app11219826
Khalifah MA, Elgendy AMA, Elgendy E. Untreated Mineralized Dentin Grafts (UMDGs) vs Xenografts Around Immediately Placed Dental Implants in the Mandibular Anterior Region: A Randomized Controlled Clinical Trial. Int J Oral Maxillofac Implants. 2024 Jun;39(3):381-8.
https://doi.org/10.11607/jomi.10584
PMid:37910831
Maeda A, Kogata S, Toyama C, Lo PC, Okamatsu C, Yamamoto R, et al. The innate cellular immune response in xenotransplantation. Frontiers in immunology. 2022;13:858604.
https://doi.org/10.3389/fimmu.2022.858604
PMid:35418992 PMCid:PMC8995651
Crapo PM, Gilbert TW, Badylak SF. An overview of tissue and whole organ decellularization processes. Biomaterials. 2011 Apr;32(12):3233-43.
https://doi.org/10.1016/j.biomaterials.2011.01.057
PMid:21296410 PMCid:PMC3084613
Perez JR, Kouroupis D, Li DJ, Best TM, Kaplan L, Correa D. Tissue Engineering and Cell-Based Therapies for Fractures and Bone Defects. Front Bioeng Biotechnol. 2018 Jul 31;6:105.
https://doi.org/10.3389/fbioe.2018.00105
PMid:30109228 PMCid:PMC6079270
Fishman JA. Prevention of infection in xenotransplantation: Designated pathogen-free swine in the safety equation. Xenotransplantation. 2020 May;27(3):e12595.
https://doi.org/10.1111/xen.12595
PMid:32495461
Fiorillo L, Cervino G, Galindo-Moreno P, Herford A, Spagnuolo G, Cicciu' M. Growth Factors in Oral Tissue Engineering: New Perspectives and Current Therapeutic Options. BioMed Research International [Internet]. 2021;2021(1):8840598.
https://doi.org/10.1155/2021/8840598
PMid:33506039 PMCid:PMC7808803
Basyuni H, Chou J, Johnston N. A scoping review of bone tissue engineering. Journal of Orthopaedic Research. 2020;38:1139-50.
Isacco CG, Nguyen KCD, Ballini A, Paduanelli G, Pham VH, Aityan SK, et al. Innovative Scaffold Solution for Bone Regeneration Made of Beta-Tricalcium Phosphate Granules, Autologous Fibrin Fold, and Peripheral Blood Stem Cells In: Duscher D, Shiffman MA, editors Regenerative Medicine and Plastic Surgery [Internet]. Cham: Springer International Publishing. 2019; 2024:167-79.
https://doi.org/10.1007/978-3-030-19962-3_13
Zheng R, Song D, Ding Y, Sun B, Lu C, Mo X, et al. A comparative study on various cell sources for constructing tissue-engineered meniscus. Front Bioeng Biotechnol. 2023 Mar 16;11:1128762.
https://doi.org/10.3389/fbioe.2023.1128762
PMid:37008037 PMCid:PMC10061001
Garcia-Aponte OF, Herwig C, Kozma B. Lymphocyte expansion in bioreactors: upgrading adoptive cell therapy. J Biol Eng. 2021 Apr 13;15(1):13.
https://doi.org/10.1186/s13036-021-00264-7
PMid:33849630 PMCid:PMC8042697
Kargozar S, Mozafari M, Hashemian SJ, Brouki Milan P, Hamzehlou S, Soleimani M, et al. Osteogenic potential of stem cells-seeded bioactive nanocomposite scaffolds: A comparative study between human mesenchymal stem cells derived from bone, umbilical cord Wharton's jelly, and adipose tissue. J Biomed Mater Res. 2018 Jan;106(1):61-72.
https://doi.org/10.1002/jbm.b.33814
PMid:27862947
Li F, Niyibizi C. Cells derived from murine induced pluripotent stem cells (iPSC) by treatment with members of TGF-beta family give rise to osteoblasts differentiation and form bone in vivo. BMC Cell Biol. 2012 Dec;13(1):35.
https://doi.org/10.1186/1471-2121-13-35
PMid:23241430 PMCid:PMC3541062
Li Y, Zhang Y, Wang H, Sun C, Liu D, Liu H, He J, Chen F, Wang W, Jiang X, Wu CT. Dental pulp mesenchymal stem cells attenuate limb ischemia via promoting capillary proliferation and collateral development in a preclinical model. Stem Cells International. 2021;2021(1):5585255.
https://doi.org/10.1155/2021/5585255
PMid:34512766 PMCid:PMC8427677
Ferraro GA, Mizuno H, Pallua N. Adipose Stem Cells: From Bench to Bedside. Stem Cells International. 2016 Jan;2016(1):6484038.
https://doi.org/10.1155/2016/6484038
PMid:27087816 PMCid:PMC4819109
Rui K, Lin X, Tian J, Wang X, Sun L, Hong X, et al. Ecto-mesenchymal stem cells: a new player for immune regulation and cell therapy. Cell Mol Immunol. 2018 Jan;15(1):82-4.
https://doi.org/10.1038/cmi.2017.69
PMid:28782759 PMCid:PMC5827180
Hong HS, Son Y. Substance-p-mobilized mesenchymal stem cells accelerate skin wound healing. Tissue Eng Regen Med. 2014 Dec 1;11(6):483-91.
https://doi.org/10.1007/s13770-014-0062-3
Fliefel R, Ehrenfeld M, Otto S. Induced pluripotent stem cells (iPSCs) as a new source of bone in reconstructive surgery: A systematic review and meta-analysis of preclinical studies. J Tissue Eng Regen Med. 2018 Jul;12(7):1780-97.
https://doi.org/10.1002/term.2697
PMid:29763985
Wuputra K, Ku CC, Wu DC, Lin YC, Saito S, Yokoyama KK. Prevention of tumor risk associated with the reprogramming of human pluripotent stem cells. J Exp Clin Cancer Res. 2020 Jun 3;39(1):100.
https://doi.org/10.1186/s13046-020-01584-0
PMid:32493501 PMCid:PMC7268627
Lagarrigue P, Soulié J, Chabrillac E, Darcos V, Grossin D, Vergez S, Combes C, Dupret-Bories A. Biomaterials and osteoradionecrosis of the jaw: Review of the literature according to the SWiM methodology. European Annals of Otorhinolaryngology, Head and Neck Diseases. 2022 Aug 1;139(4):208-15.
https://doi.org/10.1016/j.anorl.2021.06.006
PMid:34210630
Zhang Q, Wu W, Qian C, Xiao W, Zhu H, Guo J jie, et al. Advanced biomaterials for repairing and reconstruction of mandibular defects. Materials science & engineering C, Materials for biological applications. 2019;103:109858.
https://doi.org/10.1016/j.msec.2019.109858
PMid:31349473
Sánchez-Cid P, Jiménez-Rosado M, Rubio-Valle JF, Romero A, Ostos FJ, Rafii-El-Idrissi Benhnia M, et al. Biocompatible and Thermoresistant Hydrogels Based on Collagen and Chitosan. Polymers. 2022 Jan 10;14(2):272.
https://doi.org/10.3390/polym14020272
PMid:35054678 PMCid:PMC8781623
Ferreira AM, Gentile P, Chiono V, Ciardelli G. Collagen for bone tissue regeneration. Acta Biomaterialia. 2012 Sep;8(9):3191-200.
https://doi.org/10.1016/j.actbio.2012.06.014
PMid:22705634
Sukpaita T, Chirachanchai S, Pimkhaokham A, Ampornaramveth RS. Chitosan-Based Scaffold for Mineralized Tissues Regeneration. Marine Drugs. 2021 Sep 28;19(10):551.
https://doi.org/10.3390/md19100551
PMid:34677450 PMCid:PMC8540467
Sa MW, Kim JY. Effect of various blending ratios on the cell characteristics of PCL and PLGA scaffolds fabricated by polymer deposition system. Int J Precis Eng Manuf. 2013 Apr;14(4):649-55.
https://doi.org/10.1007/s12541-013-0087-x
Sun F, Sun X, Wang H, Li C, Zhao Y, Tian J, et al. Application of 3D-Printed, PLGA-Based Scaffolds in Bone Tissue Engineering. IJMS. 2022 May 23;23(10):5831.
https://doi.org/10.3390/ijms23105831
PMid:35628638 PMCid:PMC9143187
Asri R, Harun WSW, Samykano M, Lah NAC, Ghani SAC, Tarlochan F, et al. Corrosion and surface modification on biocompatible metals: A review. Materials science & engineering C, Materials for biological applications. 2017;77:1261-74.
https://doi.org/10.1016/j.msec.2017.04.102
PMid:28532004
Hanawa T. Titanium-Tissue Interface Reaction and Its Control With Surface Treatment. Frontiers in Bioengineering and Biotechnology. 2019;7:170.
https://doi.org/10.3389/fbioe.2019.00170
PMid:31380361 PMCid:PMC6650641
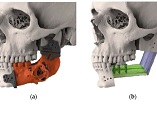
Miles BA, Potter JK, Ellis E. Computer-aided mandibular reconstruction: An analysis of available techniques. Oral and Maxillofacial Surgery Clinics of North America. 2010;22:117-33.
https://doi.org/10.1016/j.coms.2009.11.005
PMid:20159482
Chernohorskyi D, Chepurnyi Y, Vasiliev O, Voller MV, Kopchak A. Evaluation of the accuracy of surgical reconstruction of mandibular defects when using navigation templates and patient-specific titanium implants. Journal of Education, Health and Sport. 2021;11:117-32.
https://doi.org/10.12775/JEHS.2021.11.02.013
Curado TF, Silva JR, Nascimento LN, Leles JL, McKenna G, Schimmel M, Leles CR. Implant survival/success and peri‐implant outcomes of titanium‐zirconium mini implants for mandibular overdentures: results from a 1‐year randomized clinical trial. Clinical oral implants research. 2023 Aug;34(8):769-82.
https://doi.org/10.1111/clr.14102
PMid:37254798
Tarsitano A, Ciocca L, Cipriani R, Scotti R, Marchetti C. Mandibular reconstruction using computer-aided design/computer-aided manufacturing: A systematic review of outcomes. Journal of Oral and Maxillofacial Surgery. 2015;73:178-91.
Krischak GD, Gebhard F, Mohr W, Krivan V, Ignatius A, Beck A, et al. Difference in metallic wear distribution released from commercially pure titanium compared with stainless steel plates. Archives of Orthopaedic and Trauma Surgery. 2004 Mar 1;124(2):104-13.
https://doi.org/10.1007/s00402-003-0614-9
PMid:14727127
Pałka K, Pokrowiecki R. Porous Titanium Implants: A Review. Adv Eng Mater. 2018 May;20(5):1700648.
https://doi.org/10.1002/adem.201700648
Shirai T, Shimizu T, Ohtani K, Zen Y, Takaya M, Tsuchiya H. Antibacterial iodine-supported titanium implants. Acta Biomaterialia. 2011 Apr;7(4):1928-33.
https://doi.org/10.1016/j.actbio.2010.11.036
PMid:21115142
Pierrot FX, Ibarra-Gómez R, Bouquey M, Muller R, Serra C. In situ polymerization of styrene into a PMMA matrix by using an extensional flow mixing device: A new experimental approach to elaborate polymer blends. Polymer. 2017;109:160-9.
https://doi.org/10.1016/j.polymer.2016.12.045
Ibrahim AS, Badri C, Latief BS, Wijaya SK, Setiadji VS, Suwandi A. Polyetheretherketone (PEEK) for making bone implants in maxillofacial reconstruction surgery. AITI. 2017;14(2):156-67.
Zafar MS. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers. 2020;12(10):2299.
https://doi.org/10.3390/polym12102299
PMid:33049984 PMCid:PMC7599472
Hasandoost L, Rodriguez O, Alhalawani A, Zalzal P, Schemitsch EH, Waldman SD, et al. The Role of Poly(Methyl Methacrylate) in Management of Bone Loss and Infection in Revision Total Knee Arthroplasty: A Review. JFB. 2020 Apr 10;11(2):25.
https://doi.org/10.3390/jfb11020025
PMid:32290191 PMCid:PMC7353497
Kang J, Zhang J, Zheng J, Wang L, Li D, Liu S. 3D-printed PEEK implant for mandibular defects repair - a new method. Journal of the mechanical behavior of biomedical materials. 2021;116:104335.
https://doi.org/10.1016/j.jmbbm.2021.104335
PMid:33494021
Shen FH, Gasbarrini A, Lui DF, Reynolds J, Capua J, Boriani S. Integrated Custom Composite Polyetheretherketone/Carbon fiber (PEEK/CF) Vertebral Body Replacement (VBR) in the Treatment of Bone Tumors of the Spine: A Preliminary Report From a Multicenter Study. Spine. 2022 Feb 1;47(3):252-60.
https://doi.org/10.1097/BRS.0000000000004177
PMid:34310537
Deng L, He X, Xie K, Xie L, Deng Y. Dual Therapy Coating on Micro/Nanoscale Porous Polyetheretherketone to Eradicate Biofilms and Accelerate Bone Tissue Repair. Macromolecular Bioscience. 2019 Feb;19(2):1800376.
https://doi.org/10.1002/mabi.201800376
PMid:30549406
Wang X, Ma N, Feng L, Shen M, Zhou Y, Zhang X, et al. Fabrication of Bfgf/Polydopamine-Loaded Peek Implants for Improving Soft Tissue Integration by Upregulating Wnt/Β-Catenin Signaling . Rochester, NY. 2022 ;9(4):e14800.
https://doi.org/10.1016/j.heliyon.2023.e14800
PMid:37012909 PMCid:PMC10066536
Li L, Gao H, Wang C, Ji P, Huang Y, Wang C. Assessment of Customized Alveolar Bone Augmentation Using Titanium Scaffolds vs Polyetheretherketone (PEEK) Scaffolds: A Comparative Study Based on 3D Printing Technology. ACS Biomater Sci Eng. 2022 May 9;8(5):2028-39.
https://doi.org/10.1021/acsbiomaterials.2c00060
PMid:35443132
Moncayo-Matute FP, Vázquez-Silva E, Peña-Tapia PG, Torres-Jara PB, Moya-Loaiza DP, Viloria-Ávila TJ. Finite Element Analysis of Patient-Specific 3D-Printed Cranial Implant Manufactured with PMMA and PEEK: A Mechanical Comparative Study. Polymers. 2023 Sep 1;15(17):3620.
https://doi.org/10.3390/polym15173620
PMid:37688247 PMCid:PMC10490355
Stevanovic M, Selakovic D, Vasovic M, Ljujic B, Zivanovic S, Papic M, et al. Comparison of Hydroxyapatite/Poly(lactide-co-glycolide) and Hydroxyapatite/Polyethyleneimine Composite Scaffolds in Bone Regeneration of Swine Mandibular Critical Size Defects: In Vivo Study. Molecules. 2022 Mar 4;27(5):1694.
https://doi.org/10.3390/molecules27051694
PMid:35268796 PMCid:PMC8911599
Zhang P, Yang K, Zhou Z, Zhu X, Li W, Cao C, et al. Customized Borosilicate Bioglass Scaffolds With Excellent Biodegradation and Osteogenesis for Mandible Reconstruction. Front Bioeng Biotechnol. 2020 Dec 18;8:610284.
https://doi.org/10.3389/fbioe.2020.610284
PMid:33392173 PMCid:PMC7775478
Gheisari H, Karamian E, Abdellahi M. A novel hydroxyapatite -Hardystonite nanocomposite ceramic. Ceramics International. 2015 May;41(4):5967-75.
https://doi.org/10.1016/j.ceramint.2015.01.033
Filip DG, Surdu VA, Paduraru AV, Andronescu E. Current Development in Biomaterials-Hydroxyapatite and Bioglass for Applications in Biomedical Field: A Review. JFB. 2022 Nov 16;13(4):248.
https://doi.org/10.3390/jfb13040248
PMid:36412889 PMCid:PMC9680477
Li H, Ge Y, Wu Y, Jiang J, Gao K, Zhang P, et al. Hydroxyapatite coating enhances polyethylene terephthalate artificial ligament graft osseointegration in the bone tunnel. International Orthopaedics. 2011;35:1561-7.
https://doi.org/10.1007/s00264-010-1158-6
PMid:21110021 PMCid:PMC3174296
Harun W, Asri R, Alias J, Zulkifli FH, Kadirgama K, Ghani S, et al. A comprehensive review of hydroxyapatite-based coatings adhesion on metallic biomaterials. Ceramics International. 2018;44:1250-68.
https://doi.org/10.1016/j.ceramint.2017.10.162
Hirota M, Shima T, Sato I, Ozawa T, Iwai T, Ametani A, et al. Development of a biointegrated mandibular reconstruction device consisting of bone compatible titanium fiber mesh scaffold. Biomaterials. 2016 Jan;75:223-36.
https://doi.org/10.1016/j.biomaterials.2015.09.034
PMid:26513415
Manzoor F, Golbang A, Jindal S, Dixon D, McIlhagger A, Harkin-Jones E, et al. 3D printed PEEK/HA composites for bone tissue engineering applications: Effect of material formulation on mechanical performance and bioactive potential. Journal of the Mechanical Behavior of Biomedical Materials. 2021 Sep;121:104601.
https://doi.org/10.1016/j.jmbbm.2021.104601
PMid:34077906
Al-Noaman A, Rawlinson SCF. A novel bioactive glass/graphene oxide composite coating for a polyether ether ketone-based dental implant. European Journal of Oral Sciences. 2023;131(2):e12915.
https://doi.org/10.1111/eos.12915
PMid:36707252
Tahmasebi E, Alam M, Yazdanian M, Tebyanian H, Yazdanian A, Seifalian A, et al. Current biocompatible materials in oral regeneration: a comprehensive overview of composite materials. Journal of Materials Research and Technology. 2020 Sep;9(5):11731-55.
https://doi.org/10.1016/j.jmrt.2020.08.042
Park HI, Lee JH, Lee SJ. The comprehensive on-demand 3D bio-printing for composite reconstruction of mandibular defects. Maxillofac Plast Reconstr Surg. 2022 Oct 4;44(1):31.
https://doi.org/10.1186/s40902-022-00361-7
PMid:36195777 PMCid:PMC9532487
Onodera K, Miyamoto I, Hoshi I, Kawamata S, Takahashi N, Shimazaki N, Kondo H, Yamada H. Towards Optimum Mandibular Reconstruction for Dental Occlusal Rehabilitation: From Preoperative Virtual Surgery to Autogenous Particulate Cancellous Bone and Marrow Graft with Custom-Made Titanium Mesh-A Retrospective Study. Journal of Clinical Medicine. 2023 Jan 31;12(3):1122.
https://doi.org/10.3390/jcm12031122
PMid:36769770 PMCid:PMC9918119
Kazemzadeh-Narbat M, Lai BFL, Ding C, Kizhakkedathu JN, Hancock REW, Wang R. Multilayered coating on titanium for controlled release of antimicrobial peptides for the prevention of implant-associated infections. Biomaterials. 2013 Aug;34(24):5969-77.
https://doi.org/10.1016/j.biomaterials.2013.04.036
PMid:23680363
Chong E, Mobbs RJ, Pelletier MH, Walsh WR. Titanium/Polyetheretherketone Cages for Cervical Arthrodesis with Degenerative and Traumatic Pathologies: Early Clinical Outcomes and Fusion Rates. Orthopaedic Surgery. 2016;8(1):19-26.
https://doi.org/10.1111/os.12221
PMid:27028377 PMCid:PMC6584396
Dasari A, Xue J, Deb S. Magnetic nanoparticles in bone tissue engineering. Nanomaterials. 2022 Feb 24;12(5):757.
https://doi.org/10.3390/nano12050757
PMid:35269245 PMCid:PMC8911835
Selvam S, Ben Thomas M, Bhowmick T, Chandru A. Bioprinting of exosomes: Prospects and challenges for clinical applications. IJB. 2023 Feb 20;9(2):690.
https://doi.org/10.18063/ijb.690
PMid:37214319 PMCid:PMC10195394
Sun X, Yang S, Tong S, Guo S. Study on Exosomes Promoting the Osteogenic Differentiation of ADSCs in Graphene Porous Titanium Alloy Scaffolds. Front Bioeng Biotechnol. 2022 Jun 6;10:905511.
https://doi.org/10.3389/fbioe.2022.905511
PMid:35733528 PMCid:PMC9207277
Takeuchi R, Katagiri W, Endo S, Kobayashi T. Exosomes from conditioned media of bone marrow-derived mesenchymal stem cells promote bone regeneration by enhancing angiogenesis. Papaccio G, editor PLoS ONE. 2019 Nov 21;14(11):e0225472.
https://doi.org/10.1371/journal.pone.0225472
PMid:31751396 PMCid:PMC6872157
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







