Neurosurgical Complications Following Tooth Extraction: A Systematic Review and Individual Patient Meta-Analysis
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3570Keywords:
Neurosurgical Complications; Tooth Extraction; Neurosurgical Procedures; Brain Abscess; Meningitis; Cerebrovascular Accidents; Systematic Review and Meta-AnalysisAbstract
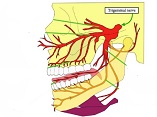
Background: We aimed to review the characteristics of patients with neurosurgical complications after tooth extraction. Materials and Methods: This systematic review followed PRISMA guidelines and searched PubMed/MEDLINE, Embase, Web of Science, and Scopus databases for studies investigating neurosurgical complications post-tooth extraction. Relevant keywords for dental extraction, adverse events or complications, and neurosurgery were searched using Boolean operators. Extracted data was synthesized using proper statistical tests. Results: Among 42 studies, 47 cases (34 males, 13 females) were included. The complications were distributed as follows: 25 brain abscesses, 11 meningitis cases, 8 cerebrovascular accidents, 2 cases with both meningitis and stroke, and 1 pituitary macroadenoma. Four deaths occurred in cerebrovascular accident cases. A significant association was found between preexisting diseases and death (odds ratio = 2.15, 95% CI: 1.08-4.29, p-value = 0.03). Three mucormycosis and two mycobacterium tuberculosis cases were reported. The most common symptoms were headache (55.32%), fever (38.3%), and laterality symptoms (25.53%). Neck pain/neck rigidity was more prevalent in females (30.77% vs. 8.82%, P = 0.042), as were nausea and vomiting (30.77% vs. 8.82%, P = 0.028). Overall, 31.91% of cases had no underlying diseases. The mean time from tooth extraction to emergency room visit was 19.73 days (SD = 31.01 days), ranging from 2 to 180 days. Fourteen cases (29.79%) involved the upper jaw, 6 (12.77%) the lower jaw, and 2 (4.26%) both jaws. Conclusion: The study introduces a novel approach by systematically reviewing and analyzing individual patient data to identify specific risk factors and symptoms associated with neurosurgical complications following tooth extraction. Healthcare providers can use the identified symptoms, such as headache and fever, as key indicators for prompt evaluation and management of patients presenting after tooth extraction, especially in male patients with pre-existing conditions who are undergoing upper jaw teeth extraction.
References
Ciobica A, Padurariu M, Curpan A, Antioch I, Chirita R, et al. Minireview on the Connections between the Neuropsychiatric and Dental Disorders: Current Perspectives and the Possible Relevance of Oxidative Stress and Other Factors. Oxid Med Cell Longev. 2020 Jun 30;2020:6702314.
https://doi.org/10.1155/2020/6702314
PMid:32685098 PMCid:PMC7345607
Wu Y, Lan Y, Mao J, Shen J, Kang T, Xie Z. The interaction between the nervous system and the stomatognathic system: from development to diseases. Int J Oral Sci. 2023 Aug 15;15(1):34.
https://doi.org/10.1038/s41368-023-00241-4
PMid:37580325 PMCid:PMC10425412
Obana M, Furuya J, Matsubara C, Tohara H, Inaji M, Miki K, Numasawa Y, Minakuchi S, Maehara T. Effect of a collaborative transdisciplinary team approach on oral health status in acute stroke patients. J Oral Rehabil. 2019 Dec;46(12):1170-1176.
https://doi.org/10.1111/joor.12855
PMid:31283027
Ruiz RL, Pattisapu JV. Combined craniomaxillofacial and neurosurgical procedures. Atlas of the Oral and Maxillofacial Surgery Clinics of North America. 2010 Sep 1;18(2):vii-i.
https://doi.org/10.1016/j.cxom.2010.08.008
PMid:21036309
Almarghlani A. Prevalence, Predictors, and Reasons for Permanent Tooth Extraction among High School Students in Saudi Arabia: A National Cross-Sectional Study. Cureus. 2022 Sep 2;14(9):e28687.
https://doi.org/10.7759/cureus.28687
Bernal-Sánchez KK, Lara-Carrillo E, Velázquez-Enriquez U, Casanova-Rosado JF, Casanova-Rosado AJ, et al. Clinical and socio-demographic factors associated with dental extractions in a clinical sample. Braz Dent J. 2023 Nov-Dec;34(6):121-129.
https://doi.org/10.1590/0103-6440202305355
PMid:38133086 PMCid:PMC10742350
Gadhia A, Pepper T. Oral Surgery, Extraction of Teeth. [Updated 2023 Jun 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
Kalenderian E, Obadan-Udoh E, Maramaldi P, Etolue J, Yansane A, Stewart D, White J, Vaderhobli R, Kent K, Hebballi NB, Delattre V, Kahn M, Tokede O, Ramoni RB, Walji MF. Classifying Adverse Events in the Dental Office. J Patient Saf. 2021 Sep 1;17(6):e540-e556.
https://doi.org/10.1097/PTS.0000000000000407
PMid:28671915 PMCid:PMC5748012
Kang F, Sah MK, Fei G. Determining the risk relationship associated with inferior alveolar nerve injury following removal of mandibular third molar teeth: A systematic review. J Stomatol Oral Maxillofac Surg. 2020 Feb;121(1):63-69.
https://doi.org/10.1016/j.jormas.2019.06.010
PMid:31476533
Kwon G, Hohman MH. Inferior Alveolar Nerve and Lingual Nerve Injury. [Updated 2023 Mar 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan.
Su N, Harroui S, Rozema F, Listl S, de Lange J, Van Der Heijden GJ. What do we know about uncommon complications associated with third molar extractions A scoping review of case reports and case series. J Korean Assoc Oral Maxillofac Surg. 2023 Feb;49(1):2-12.
https://doi.org/10.5125/jkaoms.2023.49.1.2
PMid:36859370 PMCid:PMC9985997
Gowans K, Patel M, Lewis K. Surgical Emphysema: A Rare Complication of a Simple Surgical Dental Extraction Without the Use of an Air-Driven Rotor. Dent Update. 2017 Mar;44(3):217-8, 220.
https://doi.org/10.12968/denu.2017.44.3.217
PMid:29172328
Lajolo C, Rupe C, Gioco G, Troiano G, Patini R, et al. Osteoradionecrosis of the Jaws Due to Teeth Extractions during and after Radiotherapy: A Systematic Review. Cancers (Basel). 2021 Nov 18;13(22):5798.
https://doi.org/10.3390/cancers13225798
PMid:34830954 PMCid:PMC8616343
Garcia Garcia A, Gude Sampedro F, Gandara Rey J, Gallas Torreira M. Trismus and pain after removal of impacted lower third molars. J Oral Maxillofac Surg. 1997 Nov;55(11):1223-6.
https://doi.org/10.1016/S0278-2391(97)90172-5
PMid:9371111
Yoo JH, Oh JH, Kang SH, Kim JB. Management of traumatic neuralgia in a patient with the extracted teeth and alveoloplasty: a case report. J Dent Anesth Pain Med. 2015 Dec;15(4):241-245.
https://doi.org/10.17245/jdapm.2015.15.4.241
PMid:28879286 PMCid:PMC5564161
Kroppenstedt SN, Liebig T, Mueller W, Gräf KJ, Lanksch WR, Unterberg AW. Secondary abscess formation in pituitary adenoma after tooth extraction: Case report. J Neurosurg. 2001 Feb;94(2):335-8.
https://doi.org/10.3171/jns.2001.94.2.0335
PMid:11213976
Revol P, Gleizal A, Kraft T, Breton P, Freidel M, Bouletreau P. Brain abscess and diffuse cervico-facial cellulitis: complication after mandibular third molar extraction. Revue de Stomatologie et de Chirurgie Maxillo-faciale. 2003 Oct 1;104(5):285-9.
Ghafoor H, Haroon S, Atique S, Ul Huda A, Ahmed O, Bel Khair AOM, Abdus Samad A. Neurological Complications of Local Anesthesia in Dentistry A Review. Cureus. 2023 Dec 19;15(12):e50790.
https://doi.org/10.7759/cureus.50790
Mancini A, Inchingolo AM, Blasio MD, Ruvo ED, Noia AD, Ferrante L, Vecchio GD, Palermo A, Inchingolo F, Inchingolo AD, Dipalma G. Neurological Complications following Surgical Treatments of the Lower Molars. International Journal of Dentistry. 2024;2024(1):5415597.
https://doi.org/10.1155/2024/5415597
PMid:39286455 PMCid:PMC11405104
Takkouche B, Norman G. PRISMA statement. Epidemiology. 2011 Jan 1;22(1):128.
https://doi.org/10.1097/EDE.0b013e3181fe7999
Ewald C, Kuhn S, Kalff R. Pyogenic infections of the central nervous system secondary to dental affections-a report of six cases. Neurosurg Rev. 2006;29:163-6.
https://doi.org/10.1007/s10143-005-0009-1
PMid:16501929
Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014 Jan;67(1):46-51.
https://doi.org/10.1016/j.jclinepi.2013.08.003
PMid:24035173
Amorim RP, Henriques VM, Junior FT, Reis VG, Bulhões SO. Hydrocephalus and Intracranial Hypertension by an Odontogenic Brain Abscess. Cureus. 2022 Jul 17;14(7):e26945.
https://doi.org/10.7759/cureus.26945
Nelson PB, Haverkos H, Martinez JA, Robinson AG. Abscess formation within pituitary tumors. Neurosurgery. 1983 Mar;12(3):331-3.
https://doi.org/10.1227/00006123-198303000-00016
PMid:6843806
Calderon-Miranda WG, Hernandez NE, Salazar LR, Agrawal A. Acute spontaneous subdural hematomaas unusual complication after tooth extraction. Romanian Neurosurg. 2016 Sep 15:387-90.
https://doi.org/10.1515/romneu-2016-0061
Pallesen LP, Schaefer J, Reuner U, Leonhardt H, Engellandt K, et al. Multiple brain abscesses in an immunocompetent patient after undergoing professional tooth cleaning. J Am Dent Assoc. 2014 Jun;145(6):564-8.
https://doi.org/10.14219/jada.2014.20
PMid:24878711
Hollin SA, Hayashi H, Gross SW. Intracranial abscesses of odontogenic origin. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1967 Mar 1;23(3):277-93.
https://doi.org/10.1016/0030-4220(67)90138-7
PMid:5226436
Hollin SA, Gross SW. Subdural empyema of odontogenic origin. J Mt Sinai Hosp N Y. 1964;31:540-4.
Martines F, Salvago P, Ferrara S, Mucia M, Gambino A, et al. Parietal subdural empyema as complication of acute odontogenic sinusitis: a case report. J Med Case Rep. 2014 Aug 21;8:282.
https://doi.org/10.1186/1752-1947-8-282
PMid:25146384 PMCid:PMC4145834
Andersen WC, Horton HL. Parietal lobe abscess after routine periodontal recall therapy: Report of a case. Journal of Periodontology. 1990 Apr;61(4):243-7.
https://doi.org/10.1902/jop.1990.61.4.243
PMid:2182824
Wong M, Campos-Baniak MG, Sharma V. Occipital lobe abscess following wisdom tooth extraction. Can J Ophthalmol. 2019 Jun;54(3):e145-e149.
https://doi.org/10.1016/j.jcjo.2018.08.001
PMid:31109504
Wohl TA, Kattah JC, Kolsky MP, Alper MG, Horton JC. Hemianopsia from occipital lobe abscess after dental care. Am J Ophthalmol. 1991 Dec 15;112(6):689-94.
https://doi.org/10.1016/S0002-9394(14)77276-9
PMid:1957905
Chandy B, Todd J, Stucker FJ, Nathan CA. Pott's puffy tumor and epidural abscess arising from dental sepsis: a case report. The Laryngoscope. 2001 Oct;111(10):1732-4.
https://doi.org/10.1097/00005537-200110000-00012
PMid:11801935
Cariati P, Cabello-Serrano A, Monsalve-Iglesias F, Roman-Ramos M, Garcia-Medina B. Meningitis and subdural empyema as complication of pterygomandibular space abscess upon tooth extraction. J Clin Exp Dent. 2016 Oct;8(4):e469.
https://doi.org/10.4317/jced.52916
PMid:27703619 PMCid:PMC5045698
Reddy KS, Samatha M, Sandeep N. Oral and Maxillofacial Surgery: A Rare Complication of Death Following Cavernous Sinus Thrombosis due to Maxillary Tooth Extraction. Clinical Dentistry. 2023 Mar 1;77(3): 29.
Sakashita K, Miyata K, Yamaoka A, Mikami T, Akiyama Y, et al. A case of multiple infectious intracranial aneurysms concurrently presenting with intracerebral hemorrhage and epistaxis. Interdiscip Neurosurg. 2018 Dec 1;14:93-6.
https://doi.org/10.1016/j.inat.2018.07.011
Strojnik T, Roskar Z. Brain abscess after milk tooth self-extraction. Wien Klin Wochenschr. 2004;116 Suppl 2:87-9.
Clancy U, Ronayne A, Prentice MB, Jackson A. Actinomyces meyeri brain abscess following dental extraction. BMJ Case Rep. 2015 Apr 13;2015:bcr2014207548.
https://doi.org/10.1136/bcr-2014-207548
PMid:25870213 PMCid:PMC4401930
Okada Y, Suzuki H, Ishiyama I. Fatal subarachnoid haemorrhage associated with dental local anesthesia. Aust Dent J. 1989 Aug;34(4):323-5.
https://doi.org/10.1111/j.1834-7819.1989.tb04640.x
PMid:2775019
Reddy U, Agrawal A, Hegde KV, Srikanth V, Reddy S. Massive infarction and cavernous sinus thrombosis: an uncommon complication of tooth extraction. Romanian Neurosurg. 2014 Dec 15:493-7.
Brady P, Bergin S, Cryan B, Flanagan O. Intracranial abscess secondary to dental infection. J Ir Dent Assoc. 2014; 60(1): 32-34.
Clifton TC, Kalamchi S. A case of odontogenic brain abscess arising from covert dental sepsis. Ann R Coll Surg Engl. 2012 Jan;94(1):e41-3.
https://doi.org/10.1308/003588412X13171221499667
PMid:22524927 PMCid:PMC3954226
Funakoshi Y, Hatano T, Ando M, Chihara H, Takita W, et al. Intracranial Subdural Abscess Caused by Actinomyces meyeri Related to Dental Treatment: A Case Report. NMC Case Report Journal. 2020;7(3):135-9.
https://doi.org/10.2176/nmccrj.cr.2019-0246
PMid:32695562 PMCid:PMC7363637
Yoshii T, Furudoi S, Kohjitani A, Kuwamura K, Komori T. Subdural empyema after tooth extraction in which Capnocytophaga species was isolated. Scand J Infect Dis. 2000;32(6):704-5.
https://doi.org/10.1080/003655400459702
PMid:11200389
Shibata T, Hashimoto N, Okura A, Mase M. Brain abscess of odontogenic origin in patients with malignant tumors: A report of two cases. Surg Neurol Int. 2021 Aug 16;12:417.
https://doi.org/10.25259/SNI_541_2021
PMid:34513181 PMCid:PMC8422424
Verma A, Qutab S, Baig M. Medullary brain abscess secondary to dental procedure caused by Streptococcus intermedius. BMJ Case Reports CP. 2021 Jun 1;14(6):e240769.
https://doi.org/10.1136/bcr-2020-240769
PMid:34116990 PMCid:PMC8201944
Wu PC, Tu MS, Lin PH, Chen YS, Tsai HC. Prevotella brain abscesses and stroke following dental extraction in a young patient: a case report and review of the literature. Intern Med. 2014;53(16):1881-7.
https://doi.org/10.2169/internalmedicine.53.1299
PMid:25130130
Singh H, Dua S, Goel A, Dhar A, Bhadauria V, Garg A, Katyar V, Sharma S, Shukla A. Rhino-orbital-cerebral mucormycosis in times of COVID-19: A neurosurgical experience. Surg Neurol Int. 2021 Oct 25;12:538.
https://doi.org/10.25259/SNI_772_2021
PMid:34754588 PMCid:PMC8571359
Naganawa T, Sakuma K, Kumar A, Fukuzawa S, Okamoto T, Ando T. Intracranial hemorrhage after tooth extraction in a patient with chronic disseminated intravascular coagulation. J Oral Maxillofac Surg Med Pathol. 2015 Nov 1;27(6):854-7.
https://doi.org/10.1016/j.ajoms.2015.01.014
Choi SM, Choi YJ, Kim JT, Lee SH, Park MS, et al. A case of recurrent neuro-Behçet's disease after tooth extraction. J Korean Med Sci. 2010 Jan;25(1):185-7.
https://doi.org/10.3346/jkms.2010.25.1.185
PMid:20052370 PMCid:PMC2799998
Hibberd CE, Nguyen TD. Brain abscess secondary to a dental infection in an 11-year-old child: case report. J Can Dent Assoc. 2012;78:c49.
Prabhu S, Alqahtani M, Al Shehabi M. A fatal case of rhinocerebral mucormycosis of the jaw after dental extractions and review of literature. J Infect Public Health. 2018 May-Jun;11(3):301-303.
https://doi.org/10.1016/j.jiph.2017.09.026
PMid:29107608
Hobson DTG, Imudia AN, Soto E, Awonuga AO. Pregnancy complicated by recurrent brain abscess after extraction of an infected tooth. Obstet Gynecol. 2011 Aug;118(2 Pt 2):467-470.
https://doi.org/10.1097/AOG.0b013e31822468d6
PMid:21768856
Heckmann JG, Pauli SU. Epidural abscess after dental extraction. Age and Ageing. 2015 Sep 1;44(5):901.
https://doi.org/10.1093/ageing/afv094
PMid:26259950
Chang CS, Liou CW, Huang CC, Lui CC, Chang KC. Cavernous sinus thrombosis and cerebral infarction caused by Fusobacterium nucleatum infection. Chang Gung Med J. 2004 Jun 1;27(6):459-63.
Vargas J, Hernandez M, Silvestri C, Jiménez O, Guevara N, et al. Brain abscess due to Arcanobacterium haemolyticum after dental extraction. Clin Infect Dis. 2006 Jun 15;42(12):1810-1.
https://doi.org/10.1086/504436
PMid:16705595
Ng CS, Mohamad S, Maskon O. Medical therapy of a left-sided native valve endocarditis with neurologic sequela. Saudi Med J. 2015 Jun;36(6):743.
https://doi.org/10.15537/smj.2015.6.11420
PMid:25987119 PMCid:PMC4454911
Alfano C, Chiummariello S, Dessy LA, Bistoni G, Scuderi N. Combined mucormycosis and Aspergillosis of the rhinocerebral region. In Vivo. 2006 Mar-Apr;20(2):311-5.
Nair AP, Mehrotra A, Das KK, Kumar B, Srivastav AK, et al. Calvarial tuberculosis of the parietal bone: A rare complication after dental extraction. Asian J Neurosurg. 2015 Jul-Sep;10(3):219-21.
https://doi.org/10.4103/1793-5482.161174
PMid:26396611 PMCid:PMC4553736
Corre P, Perret C, Isidor B, Khonsari RH. A brain abscess following dental extractions in a patient with hereditary hemorrhagic telangiectasia. Br J Oral Maxillofac Surg. 2011 Jul;49(5):e9-11.
https://doi.org/10.1016/j.bjoms.2010.07.014
PMid:20719417
Hayashi A, Takano T, Suzuki A, Narumiya S. Group A streptococcal brain abscess: a case report and a review of the literature since 1988. Scand J Infect Dis. 2011 Jul;43(6-7):553-5.
https://doi.org/10.3109/00365548.2011.564648
PMid:21385096
Liao Y, Wu F, Dai F, Huang Q, Feng Y, et al. Mycobacterium tuberculosis and Pseudoramibacter alactolyticus coinfection in brain after dental extraction: A case report. Medicine (Baltimore). 2019 Dec;98(50):e18289.
https://doi.org/10.1097/MD.0000000000018289
PMid:31852106 PMCid:PMC6922595
Lin GY, Yang FC, Lee JT, Wang CW. Streptococcus anginosus, tooth extraction and brain abscess. QJM. 2014 Aug;107(8):671-2.
https://doi.org/10.1093/qjmed/hct229
PMid:24334300
Al Moussawi H, Krzyzak M, Awada Z, Chalhoub JM. Streptococcus Intermedius Brain and Diverticular Abscesses After Dental Manipulation A Case Report. Cureus. 2018 Jan;10(1):e2061.
https://doi.org/10.7759/cureus.2061
Rakhshan V. Common risk factors of dry socket (alveolitis osteitis) following dental extraction: A brief narrative review. J Stomatol Oral Maxillofac Surg. 2018 Nov;119(5):407-411.
https://doi.org/10.1016/j.jormas.2018.04.011
PMid:29723658
Fragiskos FD. Surgical extraction of impacted teeth. InOral Surgery 2007 (pp. 121-179). Berlin, Heidelberg: Springer Berlin Heidelberg.
https://doi.org/10.1007/978-3-540-49975-6_7
Michael AA, Christelle DN, Leonard T, Nadia DA, Michel TNet al, Charles B. Risk factors and complications associated with dental extraction treatment in the Western Region of Cameroon: A cross sectional study. AJOHS. 2021; 8(2): 21-26.
Yamada SI, Hasegawa T, Yoshimura N, Hakoyama Y, Nitta T, et al. Prevalence of and risk factors for postoperative complications after lower third molar extraction: A multicenter prospective observational study in Japan. Medicine (Baltimore). 2022 Aug 12; 101(32):e29989.
https://doi.org/10.1097/MD.0000000000029989
PMid:35960058 PMCid:PMC9371489
Barbas N, Caplan L, Baquis G, Adelman L, Moskowitz M. Dental chair intracerebral hemorrhage. Neurology. 1987 Mar;37(3):511-2.
https://doi.org/10.1212/WNL.37.3.511
PMid:3822150
Liu J, Wu G, Jiang Y, Li L, Wang D, Liu R. Relationship Between Arterial Blood Pressure During Trigeminal Nerve Combing and Surgical Outcome in Patients with Trigeminal Neuralgia. World Neurosurg. 2020 May;137:e98-e105.
https://doi.org/10.1016/j.wneu.2020.01.038
PMid:31954896
Lapi D, Colantuoni A, Del Seppia C, Ghione S, Tonlorenzi D, et al. Persistent effects after trigeminal nerve proprioceptive stimulation by mandibular extension on rat blood pressure, heart rate and pial microcirculation. Arch Ital Biol. 2013 Mar;151(1):11-23.
https://doi.org/10.12871/00039829201312
PMid:23807620
White TG, Powell K, Shah KA, Woo HH, Narayan RK, et al. Trigeminal Nerve Control of Cerebral Blood Flow: A Brief Review. Front Neurosci. 2021 Apr 13;15:649910.
https://doi.org/10.3389/fnins.2021.649910
PMid:33927590 PMCid:PMC8076561
Popescu SM, Scrieciu M, Mercuţ V, Ţuculina M, Dascălu I. Hypertensive patients and their management in dentistry. ISRN. 2013;10: 1-8.
https://doi.org/10.5402/2013/410740
Hall GS. Anaerobic Cocci. InClinical Microbiology Procedures Handbook, Fourth Edition 2016 Jan 1 (pp. 4-13). American Society of Microbiology.
https://doi.org/10.1128/9781555818814.ch4.13
Sasmanto S, Wasito EB. Odontogenic brain abscess due to Anaerococcus prevotii infections: A case report and review article. Int J Surg Case Rep. 2022 Aug;97:107450.
https://doi.org/10.1016/j.ijscr.2022.107450
PMid:35905679 PMCid:PMC9403287
Prieto R, Callejas-Díaz A, Hassan R, de Vargas AP, López-Pájaro LF. Parvimonas micra: A potential causative pathogen to consider when diagnosing odontogenic brain abscesses. Surg Neurol Int. 2020 Jun 6; 11:140.
https://doi.org/10.25259/SNI_20_2020
PMid:32547827 PMCid:PMC7294173
Januário G, Diaz R, Nguewa P. Brain Abscess Caused by Parvimonas Micra with Successful Treatment: A Rare Case Report. FMCR. 2021;2(5):1-9.
https://doi.org/10.47746/FMCR.2021.2508
Maurer P, Hoffman E, Mast H. Bacterial meningitis after tooth extraction. Br Dent J. 2009 Jan 24;206(2):69-71.
https://doi.org/10.1038/sj.bdj.2009.3
PMid:19165261
Prasil P, Ryskova L, Plisek S, Bostik P. A rare case of purulent meningitis caused by Capnocytophaga canimorsus in the Czech Republic - case report and review of the literature. BMC Infect Dis. 2020 Feb 3;20(1):100.
https://doi.org/10.1186/s12879-020-4760-2
PMid:32013874 PMCid:PMC6998360
Le Moal G, Landron C, Grollier G, Robert R, Burucoa C. Meningitis due to Capnocytophaga canimorsus after receipt of a dog bite: case report and review of the literature. Clin Infect Dis. 2003 Feb 1;36(3):e42-6.
https://doi.org/10.1086/345477
PMid:12539089
Rohit S, Reddy P. Efficacy of postoperative prophylactic antibiotic therapy in third molar surgery. Journal of Clinical and Diagnostic Research: JCDR. 2014 May;8(5): 14.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







