Comparison of Tensile Strengths of Synthetic and Natural Absorbable Sutures in Minor Oral Surgeries: A Randomized Clinical Trial
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3621Keywords:
Chromic Catgut; Polyglycolic Acid; Tensile Strength; Oral Surgery; SuturesAbstract
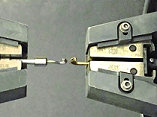
Background: Proper suture selection is important in oral surgery for uncomplicated healing. This study was conducted to compare the tensile strength of two absorbable natural and artificial sutures in minor oral surgeries. Materials and Methods: In this randomized clinical trial study, two types of absorbable sutures, 0-4 Chromic catgut and Polyglycolic Acid (PGA) were randomly used in minor oral surgery in 16 systemically healthy patients. Tensile strength tests were performed for one part of the suture thread before suturing along with sutures removed on days 7 and 10 post-surgery (24 suture threads for each group). Suture parts were tested by a Universal Testing Machine for tensile strength. Results: The mean tensile strength of chromic catgut suture on day 0 was )10.40±1.61 N), 7th day (8.76±1.66 N), and 10th day )6.45±1.14 N). The mean tensile strength of the PGA suture thread on day 0 was (16.82±2.94 N), 7th (14.56±2.66 N), and 10th day (11.50±2.15 N). The mean tensile strength of the PGA suture was significantly higher at baseline, 7 and 10 days after surgery compared to the absorbable chromic catgut suture (p<0.001). In chromic catgut sutures and PGA sutures, the mean tensile strength on day 10 was significantly lower than on days 7 (p<0.05) and 0 days (p<0.001), and the mean tensile strength on day 7 was significantly lower than on day 0 (p<0.05). Conclusion: The results indicate that PGA sutures maintain significantly higher tensile strength compared to chromic catgut sutures throughout the post-surgical period. This suggests that PGA sutures may be more suitable for minor oral surgeries where higher tensile strength is required for optimal wound healing. Surgeons should consider the specific needs of the surgical site and the duration of healing when selecting the appropriate suture material.
References
Anushya P, Ganesh SB, Jayalakshmi S. Evaluation of tensile strength of surgical absorbable and nonabsorbable suture materials after immersion in different fruit juices: An in vitro study. J Adv Pharm Technol Res. 2022; 13:108-11.
https://doi.org/10.4103/japtr.japtr_267_22
PMid:36643124 PMCid:PMC9836114
Faris A, Khalid L, Hashim M, Yaghi S, Magde T, Bouresly W, Hamdoon Z, Uthman AT, Marei H, Al-Rawi N. Characteristics of suture materials used in oral surgery: systematic review. international dental journal. 2022 Jun 1;72(3):278-87.
https://doi.org/10.1016/j.identj.2022.02.005
PMid:35305815 PMCid:PMC9275112
Saravanakumar R, Mathew M, Balu P, Ilangovan K, Reddy V, Devi S. Evaluation of Tensile Strength of Surgical Absorbable and Non-Absorbable Suture Materials-An In vitro Study. SBV Journal of Basic, Clinical and Applied Health Science. 2018; 2:111-116.
https://doi.org/10.5005/jp-journals-10082-01134
O'Neal R, Alleyn C. Suture materials and techniques. Curr Opin Periodontol. 1997; 4:89-95.
Huang T-W, Cheng P-W, Chan Y-H, Wang C-T, Fang K-M, Young T-H. Clinical and biomechanical analyses to select a suture material for uvulopalatopharyngeal surgery. Otolaryngol Head Neck Surg. 2010; 143(5):655-61.
https://doi.org/10.1016/j.otohns.2010.06.919
PMid:20974335
Varma SR, Jaber M, Aboufanas S, Thomas S, Al Hujailan RG, Al Qaoud SK. Evaluating tensile strengths of absorbable suture materials in herbal solutions: An In vitro study. J Int Oral Health. 2019; 11(3):148-52.
https://doi.org/10.4103/jioh.jioh_79_19
Chu C. The degradation and biocompatibility of suture materials. Biocompatibility of tissue analogs. 1985; 1:261-322.
Briddell JW, Riexinger LE, Graham J, Ebenstein DM. Comparison of Artificial Saliva vs Saline Solution on Rate of Suture Degradation in Oropharyngeal Surgery. JAMA Otolaryngol Head Neck Surg. 2018; 144(9):824-30.
https://doi.org/10.1001/jamaoto.2018.1441
PMid:30128560 PMCid:PMC6233633
Newman J, George J, Shepherd J, Klika A, Higuera C, Krebs V. Effects of Topical Antiseptic Solutions Used During Total Knee Arthroplasty on Suture Tensile Strength. Surg Technol Int. 2017; 30:399-404.
Kim JC, Lee YK, Lim BS, Rhee SH, Yang HC. Comparison of tensile and knot security properties of surgical sutures. J Mater Sci Mater Med. 2007; 18(12):2363-9.
https://doi.org/10.1007/s10856-007-3114-6
PMid:17569012
Nindhia TG, Putu Astawa I, Nindhia TS. Comparison tensile strength of natural and synthetic absorbable sutures. Int J Appl Pharmaceutics. 2019;11(5):157-9.
https://doi.org/10.22159/ijap.2019.v11s5.T1011
Fomete B, Saheeb BD, Obiadazie AC. A prospective clinical evaluation of the longevity of resorbable sutures in oral surgical procedures. Niger J Clin Pract. 2013; 16(3):334-8.
https://doi.org/10.4103/1119-3077.113457
PMid:23771456
Khiste SV, Ranganath V, Nichani AS. Evaluation of tensile strength of surgical synthetic absorbable suture materials: an in vitro study. J Periodontal Implant Sci. 2013; 43(3):130-5.
https://doi.org/10.5051/jpis.2013.43.3.130
PMid:23837127 PMCid:PMC3701834
Shaw RJ, Negus TW, Mellor TK. A prospective clinical evaluation of the longevity of resorbable sutures in oral mucosa. Br J Oral Maxillofac Surg. 1996; 34(3):252-4.
https://doi.org/10.1016/S0266-4356(96)90280-6
PMid:8818261
Abellلn D, Nart J, Pascual A, Cohen RE, Sanz-Moliner JD. Physical and mechanical evaluation of five suture materials on three-knot configurations: An in vitro study. Polymers. 2016; 8(4):147.
https://doi.org/10.3390/polym8040147
PMid:30979247 PMCid:PMC6432448
Byrne M, Aly A. The Surgical Suture. Aesthet Surg J. 2019 Mar;39(Suppl_2):S67-S72.
https://doi.org/10.1093/asj/sjz036
PMid:30869751
Chung E, McPherson N, Grant A. Tensile strength of absorbable suture materials: in vitro analysis of the effects of pH and bacteria. J Surg Educ. 2009; 66(4):208-11.
https://doi.org/10.1016/j.jsurg.2009.06.007
PMid:19896625
Selvig KA, Biagiotti GR, Leknes KN, Wikesjِ UM. Oral tissue reactions to suture materials. Int J Periodontics Restorative Dent. 1998; 18(5):474-87.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







