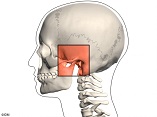
A comparative study of the application of PBM therapy in the treatment of temporomandibular joint diseases (TMD)
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3644Keywords:
Photobiomodulation; Temporomandibular Disorder (TMD); Quality of LifeAbstract
Background: The primary objective of this trial was to evaluate the supplementary effect of photobiomodulation when added to orofacial myofunctional therapy on symptoms of Temporomandibular Disorder (TMD) in TMD. Materials and Methods: This pilot randomized trial investigated the effects of photobiomodulation on TMD symptoms. Eleven women with mild to moderate TMD were randomly assigned to either an experimental group (EG, n=5) receiving photobiomodulation combined with orofacial myofunctional therapy or a control group (CG, n=6) receiving passive orofacial myofunctional treatment alone. Participants underwent 12 sessions of treatment, with photobiomodulation administered using an 830nm laser at 48J/cm2 fluence. Outcome measures included pain levels and oral health-related quality of life. Results: The experimental group had considerably greater readings for all motions, including protrusion (P=0.037), sides (P=0.0025; P=0.0014), and opening (P=0.039), according to an examination of the groups. The control group’s findings were statistically significant only for the measurements on the left and right (P=0.0030 and 0.0026, respectively). Numerous traits associated with mandibular mobility showed a discernible improvement before and after therapy in the EG. These variables include noise at the right and left temporomandibular joint (TMJ) during opening and closing of the mouth (P=0.019), noise at the right and left TMJ during protrusion (P=0.147; P=0.049), noise at the right and left TMJ during opening of the mouth (P=0.028; P=0.038), and noise at the left TMJ during opening of the mouth (P=0.012). There was only a reduction in left-sided pain (P=0.019) for the control group when comparing mandibular movements before and after treatment. Conclusion: In conclusion, photobiomodulation treatment improved orofacial myofunctional therapy results, which increased speech therapy’s efficacy in treating temporomandibular disorders.
References
Xu GZ, Jia J, Jin L, Li JH, Wang ZY, Cao DY. Low-level laser therapy for temporomandibular disorders: a systematic review with meta-analysis. Pain Res Manag. 2018;2018:4230583.
https://doi.org/10.1155/2018/4230583
PMid:29861802 PMCid:PMC5971344
Ferreira CLP, Machado BC, Borges CG, Rodrigues Da Silva MA, Sforza C, De Felício CM. Impaired orofacial motor functions on chronic temporomandibular disorders. J Electromyogr Kinesiol. 2014;24(4):56571.
https://doi.org/10.1016/j.jelekin.2014.04.005
PMid:24816190
Figueiredo VMG, Cavalcanti AL, Farias ABL, Nascimento SR. Prevalência de sinais, sintomas e fatores associados em portadores de disfunção temporomandibular. Acta Scientiarum Health Science. 2009;31(2):159-63.
https://doi.org/10.4025/actascihealthsci.v31i2.5920
Felício CM. Desordens temporomandibulares: terapia fonoaudiológica. In: Felício CM, Trawitzki LVV Interfaces da medicina, odontologia e fonoaudiologia no complexo cérvico-craniofacial. Barueri: Pro-Fono. 2009;9:177-98.
Özköylü, G., Saraç, D., Sasany, R. et al. Comparison of monoblock and twinblock mandibular advancement devices in patiens with obstructive sleep apnea and temporomandibular disorder: effects on airway volume, polysomnography parameters, and sleepiness scale scores. BMC Oral Health 24, 1026 (2024).
https://doi.org/10.1186/s12903-024-04653-4
PMid:39215302 PMCid:PMC11365127
Costa SAP, Florezi GP, Artes GE, Costa JRD, Gallo RT, Freitas PM, et al. The analgesic effect of photobiomodulation therapy (830 nm) on the masticatory muscles: a randomized, double-blind study. Braz Oral Res. 2017;31:e107.
https://doi.org/10.1590/1807-3107bor-2017.vol31.0107
Borges RMM, Cardoso DS, Flores BC, da Luz RD, Machado CR, Cerveira GP, et al. Effects of different photobiomodulation dosimetries on temporomandibular dysfunction: a randomized, double-blind, placebocontrolled clinical trial. Lasers Med Sci. 2018;33(9):1859-66.
https://doi.org/10.1007/s10103-018-2533-6
PMid:29850961
Batista SL, et al. Amplitude oral e dor orofacial em pacientes com disfunção temporomandibular submetidos a laserterapia e a terapia miofuncional orofacial. Rev Bras Ciênc Saúde. 2019(Supl.):85-94.
Matias AGC, Rocha AB, Santos CS, Fonseca MA. Modulação da dor em portadores de disfunções temporomandibular pela ação do laser AsGaAL. Interscientia. 2014;2(2):25-37.
Kuroiwa DN, Marinelli JG, Rampani MS, Oliveira W, Nicodemo D. Desordens temporomandibulares e dor orofacial: estudo da qualidade de vida medida pelo Medical Outcomes Study 36 - Item Short Form Health Survey*. Rev Dor [online]. 2011;12(2):93-8.
https://doi.org/10.1590/S1806-00132011000200003
Dahlström L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life A systematic review. Acta Odontol Scand. 2010;68(2):80-5.
https://doi.org/10.3109/00016350903431118
PMid:20141363
Sancakli E, Gokcen-Rohlig B, Balik A, Ongul D, Kipirdi S, Keskin H. Early results of low-level laser application for masticatory muscle pain: a double-blind randomized clinical study. BMC Oral Health. 2015;15(1):131.
https://doi.org/10.1186/s12903-015-0116-5
PMid:26496720 PMCid:PMC4619518
Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6(4):301-55.
Oliveira BH, Nadanovsky P. Psychometric properties of the Brazilian version of the Oral Health Impact Profile-short form. Community Dent Oral Epidemiol. 2005;33(4):307-14.
https://doi.org/10.1111/j.1600-0528.2005.00225.x
PMid:16008638
Dias WCFGDS, Cavalcanti RVA, Magalhães Júnior HV, Pernambuco LDA, Alves GÂDS. Effects of photobiomodulation combined with orofacial myofunctional therapy on the quality of life of individuals with temporomandibular disorder. In CoDAS. 2022; 34:e20200313. Sociedade Brasileira de Fonoaudiologia.
https://doi.org/10.1590/2317-1782/20212020313
PMid:35416889 PMCid:PMC9886175
Alves GÂDS, Gondim YRDR, Lima JASD, Silva MAPD, Florêncio DSF, Almeida LNAD, et al. Effects of photobiomodulation associated with orofacial myofactional therapy on temporomandibular joint dysfunction. In CoDAS. 2021;33:e20200193.
https://doi.org/10.1590/2317-1782/20202020193
PMid:34105614
Altuhafy M, Ahmed S, Jabr L, Khan J. Effectiveness of photobiomodulation and orofacial myofunctional therapy in orofacial pain disorders A systematic review of randomized control trials. Lasers in Medical Science. 2024 May 9;39(1):127.
https://doi.org/10.1007/s10103-024-04073-4
PMid:38722392
Hanna R, Dalvi S, Bensadoun RJ, Benedicenti S. Role of photobiomodulation therapy in modulating oxidative stress in temporomandibular disorders A systematic review and meta-analysis of human randomised controlled trials. Antioxidants. 2021 Jun 25;10(7):1028.
https://doi.org/10.3390/antiox10071028
PMid:34202292 PMCid:PMC8300797
Farshidfar N, Farzinnia G, Samiraninezhad N, Assar S, Firoozi P, Rezazadeh F, et al. The effect of Photobiomodulation on temporomandibular pain and functions in patients with temporomandibular disorders: an updated systematic review of the current randomized controlled trials. Journal of lasers in medical sciences. 2023;14:e24.
https://doi.org/10.34172/jlms.2023.24
PMid:37744015 PMCid:PMC10517581
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







