Robotic Assist and Virtual Surgical Planning in Orthognathic Surgery
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3672Keywords:
Virtual Surgical Planning (VSP); Robotic Assistance; Orthognathic Surgery; Surgical PrecisionAbstract
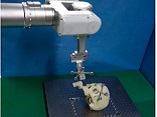
Orthognathic surgery, critical for correcting jaw deformities and improving facial function and aesthetics, has undergone transformative changes with the introduction of robotic assistance and Virtual Surgical Planning (VSP). These technologies have revolutionized the field by enhancing precision, reducing operative times, and enabling more predictable surgical outcomes. Robotic systems, including the Da Vinci® and ROSA® platforms, provide sub-millimeter precision in osteotomies, while VSP enables comprehensive preoperative planning by integrating advanced 3D imaging and simulation techniques. Together, these technologies provide an unparalleled level of control and precision in surgical procedures, significantly enhancing patient outcomes. Major advancements in the field include the integration of artificial intelligence and machine learning into surgical planning, which allows for better prediction of postoperative outcomes and real-time adjustments during surgery. Augmented reality is also gaining traction as a tool for intraoperative guidance, further enhancing the precision of robotic-assisted procedures. Emerging technologies such as haptic feedback systems and next-generation robotic arms hold promise for even greater improvements in surgical accuracy and efficiency. The relevance of these technologies to clinical practice is profound. By reducing complications, enhancing accuracy, and improving both functional and aesthetic results, robotic assistance and VSP are redefining standards in orthognathic surgery. However, barriers related to cost, surgeon training, and infrastructure must be addressed to enable the widespread adoption of these technologies. Future research should focus on validating these technologies in large-scale clinical trials and assessing their long-term benefits and cost-effectiveness. Ultimately, the integration of these cutting-edge technologies has the potential to revolutionize orthognathic surgery, making it safer, more efficient, and more personalized for patients.
References
Kim JY, Lee YC, Kim SG, Garagiola U. Advancements in Oral Maxillofacial Surgery: A Comprehensive Review on 3D Printing and Virtual Surgical Planning. Appl Sci. 2023 Sep 1;13(17):9907.
https://doi.org/10.3390/app13179907
Zinser MJ, Sailer HF, Ritter L, Braumann B, Maegele M, Zöller JE. A Paradigm Shift in Orthognathic Surgery? A Comparison of Navigation, Computer-Aided Designed/Computer-Aided Manufactured Splints, and "Classic" Intermaxillary Splints to Surgical Transfer of Virtual Orthognathic Planning. J Oral Maxillofac Surg. 2013 Dec;71(12):2151.e1.
https://doi.org/10.1016/j.joms.2013.07.007
PMid:24237776
Chin SJ, Wilde F, Neuhaus M, Schramm A, Gellrich NC, Rana M. Accuracy of virtual surgical planning of orthognathic surgery with aid of CAD/CAM fabricated surgical splint-A novel 3D analyzing algorithm. J Cranio-Maxillofac Surg. 2017 Dec;45(12):1962-70.
https://doi.org/10.1016/j.jcms.2017.07.016
PMid:29066041
Woo SY, Lee SJ, Yoo JY, Han JJ, Hwang SJ, Huh KH, et al. Autonomous bone reposition around anatomical landmark for robot-assisted orthognathic surgery. J Cranio-Maxillofac Surg. 2017 Dec;45(12):1980-8.
https://doi.org/10.1016/j.jcms.2017.09.001
PMid:29042168
Wu J, Hui W, Chen S, Niu J, Lin Y, Luan N, et al. Error Analysis of Robot-Assisted Orthognathic Surgery. J Craniofac Surg. 2020 Nov;31(8):2324-8.
https://doi.org/10.1097/SCS.0000000000006767
PMid:33136882
Lin HH, Chang HW, Wang CH, Kim SG, Lo LJ. Three-Dimensional Computer-Assisted Orthognathic Surgery: Experience of 37 Patients. Ann Plast Surg. 2015 May;74:S118-26.
https://doi.org/10.1097/SAP.0000000000000455
PMid:25785379
Dekker PK, Fleury CM, Abdou SA, Charipova K, Eze VC, James NER, et al. A Look Back: A Single Surgeon's Experience Using Virtual Surgical Planning in Adult Orthognathic Surgery. J Craniofac Surg. 2022 Oct;33(7):2005-10.
https://doi.org/10.1097/SCS.0000000000008677
PMid:36201697
Stokbro K, Aagaard E, Torkov P, Bell RB, Thygesen T. Virtual planning in orthognathic surgery. Int J Oral Maxillofac Surg. 2014 Aug;43(8):957-65.
https://doi.org/10.1016/j.ijom.2014.03.011
PMid:24746388
Farrell BB, Franco PB, Tucker MR. Virtual Surgical Planning in Orthognathic Surgery. Oral Maxillofac Surg Clin N Am. 2014 Nov;26(4):459-73.
https://doi.org/10.1016/j.coms.2014.08.011
PMid:25246324
Ho CT, Denadai R, Lo LJ, Lin HH. Average 3D skeletofacial model as a template for maxillomandibular repositioning during virtual orthognathic surgical planning. Plast Reconstr Surg. 2023 Mar 21:10-97.
https://doi.org/10.1097/PRS.0000000000010449
PMid:36940142
Zhang N, Liu S, Hu Z, Hu J, Zhu S, Li Y. Accuracy of virtual surgical planning in two-jaw orthognathic surgery: comparison of planned and actual results. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016 Aug;122(2):143-51.
https://doi.org/10.1016/j.oooo.2016.03.004
PMid:27209483
Naini FB. Historical evolution of orthognathic surgery. Orthognathic surgery: principles, planning and practice. 2016 Dec 16:23-82.
https://doi.org/10.1002/9781119004370.ch2
Alkhayer A, Piffkó J, Lippold C, Segatto E. Accuracy of virtual planning in orthognathic surgery: a systematic review. Head Face Med. 2020 Dec;16(1):34.
https://doi.org/10.1186/s13005-020-00250-2
PMid:33272289 PMCid:PMC7716456
Hullihen SP. Case of Elongation of the under Jaw and Distortion of the Face and Neck, Caused by a Burn, Successfully Treated. Am J Dent Sci. 1849 Jan;9(2):157-65.
Fillies T, Seier T. History of Orthognathic Surgery. InFundamentals of Craniofacial Malformations: Vol. 2, Treatment Principles 2023 Nov 1 (pp. 125-130). Cham: Springer International Publishing.
https://doi.org/10.1007/978-3-031-28069-6_10
Nadjmi N, Mollemans W, Daelemans A, Van Hemelen G, Schutyser F, Bergé S. Virtual occlusion in planning orthognathic surgical procedures. Int J Oral Maxillofac Surg. 2010 May;39(5):457-62.
https://doi.org/10.1016/j.ijom.2010.02.002
PMid:20226628
Kadam D. Professor Hugo Lorenz Obwegeser (1920-2017): An Icon of Orthognathic Surgery. Indian J Plast Surg. 2023 Oct;56(05):393-4.
https://doi.org/10.1055/s-0043-1776312
PMid:38026772 PMCid:PMC10680991
Anderson P, Yong R, Surman T, Rajion Z, Ranjitkar S. Application of three‐dimensional computed tomography in craniofacial clinical practice and research. Aust Dent J. 2014 Jun;59(s1):174-85.
https://doi.org/10.1111/adj.12154
PMid:24611727
Lee KJC, Tan SL, Tan DBP, Yong CW, Chew MT. Accuracy of a digital workflow for bimaxillary orthognathic surgery: comparison of planned and actual outcomes. Int J Comput Dent. 2022 Nov 25;25(4):397-405.
Bennici O, Malgioglio A, Moschitto S, Spagnuolo G, Lucchina AG, Ronsivalle V, et al. A Full Computerized Workflow for Planning Surgically Assisted Rapid Palatal Expansion and Orthognathic Surgery in a Skeletal Class III Patient. Jeng JH, editor. Case Rep Dent. 2022 Oct 19;2022:1-18.
https://doi.org/10.1155/2022/6413898
PMid:36312572 PMCid:PMC9605851
Awad D, Reinert S, Kluba S. Accuracy of Three-Dimensional Soft-Tissue Prediction Considering the Facial Aesthetic Units Using a Virtual Planning System in Orthognathic Surgery. J Pers Med. 2022 Aug 25;12(9):1379.
https://doi.org/10.3390/jpm12091379
PMid:36143164 PMCid:PMC9503557
Sodergren MH, Darzi A. Robotic cancer surgery. J Br Surg. 2013 Jan 1;100(1):3-4.
https://doi.org/10.1002/bjs.8972
PMid:23132653
Li T, Badre A, Alambeigi F, Tavakoli M. Robotic Systems and Navigation Techniques in Orthopedics: A Historical Review. Appl Sci. 2023 Aug 29;13(17):9768.
https://doi.org/10.3390/app13179768
Rivero-Moreno Y, Echevarria S, Vidal-Valderrama C, Pianetti L, Cordova-Guilarte J, Navarro-Gonzalez J, et al. Robotic surgery: a comprehensive review of the literature and current trends. Cureus. 2023 Jul;15(7).
https://doi.org/10.7759/cureus.42370
PMid:37621804 PMCid:PMC10445506
Pillai A, Ratnathankom A, Ramachandran SN, Udayakumaran S, Subhash P, Krishnadas A. Expanding the spectrum of robotic assistance in cranial neurosurgery. Oper Neurosurg. 2019;17(2):164-73.
https://doi.org/10.1093/ons/opy229
PMid:30203040
Biswas P, Sikander S, Kulkarni P. Recent advances in robot-assisted surgical systems. Biomed Eng Adv. 2023;100109.
https://doi.org/10.1016/j.bea.2023.100109
Ebeling M, Scheurer M, Sakkas A, Wilde F, Schramm A. First-Hand Experience and Result with New Robot-Assisted Laser LeFort-I Osteotomy in Orthognathic Surgery: A Case Report. J Pers Med. 2023 Feb 3;13(2):287.
https://doi.org/10.3390/jpm13020287
PMid:36836521 PMCid:PMC9962026
Borumandi F, Heliotis M, Kerawala C, Bisase B, Cascarini L. Role of robotic surgery in oral and maxillofacial, and head and neck surgery. Br J Oral Maxillofac Surg. 2012 Jul;50(5):389-93.
https://doi.org/10.1016/j.bjoms.2011.06.008
PMid:21802802
Liu HH, Li LJ, Shi B, Xu CW, Luo E. Robotic surgical systems in maxillofacial surgery: a review. Int J Oral Sci. 2017 Jun;9(2):63-73.
https://doi.org/10.1038/ijos.2017.24
PMid:28660906 PMCid:PMC5518975
Stefanelli LV, Mandelaris GA, Franchina A, Di Nardo D, Galli M, Pagliarulo M, et al. Accuracy Evaluation of 14 Maxillary Full Arch Implant Treatments Performed with Da Vinci Bridge: A Case Series. Materials. 2020 Jun 22;13(12):2806.
https://doi.org/10.3390/ma13122806
PMid:32580340 PMCid:PMC7344455
Elsabeh R, Singh S, Shasho J, Saltzman Y, Abrahams JM. Cranial neurosurgical robotics. Br J Neurosurg. 2021 Sep 3;35(5):532-40.
https://doi.org/10.1080/02688697.2021.1950622
PMid:34355992
Han JJ, Woo SY, Yi WJ, Hwang SJ. A Robot Arm and Image-Guided Navigation Assisted Surgical System for Maxillary Repositioning in Orthognathic Surgery: A Phantom Skull-Based Trial. Appl Sci. 2020 Feb 24;10(4):1549.
https://doi.org/10.3390/app10041549
Starch-Jensen T, Hernández-Alfaro F, Kesmez Ö, Gorgis R. Accuracy of Orthognathic Surgical Planning using Three-dimensional Virtual Techniques compared with Conventional Two-dimensional Techniques: a Systematic Review. J Oral Maxillofac Res. 2023 Mar;14(1):e1.
https://doi.org/10.5037/jomr.2023.14101
Schneider D, Kämmerer PW, Hennig M, Schön G, Thiem DGE, Bschorer R. Customized virtual surgical planning in bimaxillary orthognathic surgery: a prospective randomized trial. Clin Oral Investig. 2019 Jul 1;23(7):3115-22.
https://doi.org/10.1007/s00784-018-2732-3
PMid:30443778
Otranto De Britto Teixeira A, Almeida MADO, Almeida RCDC, Maués CP, Pimentel T, Ribeiro DPB, et al. Three-dimensional accuracy of virtual planning in orthognathic surgery. Am J Orthod Dentofacial Orthop. 2020 Nov;158(5):674-83.
https://doi.org/10.1016/j.ajodo.2019.09.023
PMid:33008712
Ha SH, Youn SM, Kim CY, Jeong CG, Choi JY. Surgical Accuracy of 3D Virtual Surgery and CAD/CAM-Assisted Orthognathic Surgery for Skeletal Class III Patients. J Craniofac Surg. 2023 Jan;34(1):96-102.
https://doi.org/10.1097/SCS.0000000000008980
PMid:36044286
Marlière DAA, Demétrio MS, Schmitt ARM, Lovisi CB, Asprino L, Chaves-Netto HD de M. Accuracy between virtual surgical planning and actual outcomes in orthognathic surgery by iterative closest point algorithm and color maps: A retrospective cohort study. Med Oral Patol Oral Cir Bucal. 2019 Mar;24(2):e243.
https://doi.org/10.4317/medoral.22724
PMid:30818318 PMCid:PMC6441591
Elshebiny T, Morcos S, Mohammad A, Quereshy F, Valiathan M. Accuracy of Three-Dimensional Soft Tissue Prediction in Orthognathic Cases Using Dolphin Three-Dimensional Software. J Craniofac Surg. 2019 Mar;30(2):525-8.
https://doi.org/10.1097/SCS.0000000000005037
PMid:30358749
Resnick CM, Inverso G, Wrzosek M, Padwa BL, Kaban LB, Peacock ZS. Is There a Difference in Cost Between Standard and Virtual Surgical Planning for Orthognathic Surgery? J Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg. 2016 Sep;74(9):1827-33.
https://doi.org/10.1016/j.joms.2016.03.035
PMid:27181623
Steinhuber T, Brunold S, Gärtner C, Offermanns V, Ulmer H, Ploder O. Is Virtual Surgical Planning in Orthognathic Surgery Faster Than Conventional Planning? A Time and Workflow Analysis of an Office-Based Workflow for Single- and Double-Jaw Surgery. J Oral Maxillofac Surg. 2018 Feb 1;76(2):397-407.
https://doi.org/10.1016/j.joms.2017.07.162
PMid:28826783
Jaiswal MS, Hwang DS. Clinical Analysis of Patients who Underwent Reoperation After Orthognathic Surgery: A 14-Year Retrospective Study. J Craniofac Surg. 2023 Dec;34(8):e781.
https://doi.org/10.1097/SCS.0000000000009655
Kesmez Ö, Valls-Ontañón A, Starch-Jensen T, Haas-Junior Ol, Hernández-Alfaro F. Virtual surgical planning in orthognathic surgery with the use of patient-specific plates compared with conventional plates. A systematic review focusing on complications, financial expenses, professional and patient-reported outcome measures. Med Oral Patol Oral Cirugia Bucal. 2022;e507-17.
https://doi.org/10.4317/medoral.25424
PMid:36173724 PMCid:PMC9648647
Tran NH, Tantidhnazet S, Raocharernporn S, Kiattavornchareon S, Pairuchvej V, Wongsirichat N. Accuracy of Three-Dimensional Planning in Surgery-First Orthognathic Surgery: Planning Versus Outcome. J Clin Med Res. 2018;10(5):429-36.
https://doi.org/10.14740/jocmr3372w
PMid:29581806 PMCid:PMC5862091
Chen J, Abousy M, Girard A, Duclos O, Patel V, Jenny H, et al. The Impact of Virtual Surgical Planning on Orthognathic Surgery: Contributions From Two Specialties. J Craniofac Surg. 2022 Jul;33(5):1418-23.
https://doi.org/10.1097/SCS.0000000000008607
PMid:35258010
Hanafy M, Akoush Y, Abou-ElFetouh A, Mounir RM. Precision of orthognathic digital plan transfer using patient-specific cutting guides and osteosynthesis versus mixed analogue-digitally planned surgery: a randomized controlled clinical trial. Int J Oral Maxillofac Surg. 2020 Jan;49(1):62-8.
https://doi.org/10.1016/j.ijom.2019.06.023
PMid:31262680
Guo Y, Xu W, Tu P, Han J, Zhang C, Liu J, et al. Design and implementation of a surgical planning system for robotic assisted mandible reconstruction with fibula free flap. Int J Comput Assist Radiol Surg. 2022 Dec 1;17(12):2291-303.
https://doi.org/10.1007/s11548-022-02748-3
PMid:36166164
Kong X, Duan X, Wang Y. An integrated system for planning, navigation and robotic assistance for mandible reconstruction surgery. Intell Serv Robot. 2016 Apr 1;9(2):113-21.
https://doi.org/10.1007/s11370-015-0189-7
Ying X, Tian K, Zhang K, Ma X, Guo H. Accuracy of virtual surgical planning in segmental osteotomy in combination with bimaxillary orthognathic surgery with surgery first approach. BMC Oral Health. 2021 Dec;21(1):529.
https://doi.org/10.1186/s12903-021-01892-7
PMid:34654418 PMCid:PMC8518167
Valls-Ontañón A, Ascencio-Padilla RDJ, Vela-Lasagabaster A, Sada-Malumbres A, Haas-Junior OL, Masià-Gridilla J, et al. Relevance of 3D virtual planning in predicting bony interferences between distal and proximal fragments after sagittal split osteotomy. Int J Oral Maxillofac Surg. 2020 Aug;49(8):1020-8.
https://doi.org/10.1016/j.ijom.2019.12.001
PMid:31918988
Liang J, Li Q, Wang X, Liu XJ. Prospect of Robot Assisted Maxilla-Mandibula-Complex Reposition in Orthognathic Surgery. In2022 IEEE International Conference on Robotics and Biomimetics (ROBIO) 2022 Dec 5 (pp. 1745-1750). IEEE.
https://doi.org/10.1109/ROBIO55434.2022.10011845
PMid:35399707 PMCid:PMC8990433
Han JJ, Woo SY, Yi WJ, Hwang SJ. Robot-Assisted Maxillary Positioning in Orthognathic Surgery: A Feasibility and Accuracy Evaluation. J Clin Med. 2021 Jun 11;10(12):2596.
https://doi.org/10.3390/jcm10122596
PMid:34208399 PMCid:PMC8231103
Lawrie L, Gillies K, Duncan E, Davies L, Beard D, Campbell MK. Barriers and enablers to the effective implementation of robotic assisted surgery. Srinivasan R, editor. PLOS ONE. 2022 Aug 29;17(8):e0273696.
https://doi.org/10.1371/journal.pone.0273696
PMid:36037179 PMCid:PMC9423619
Prewitt R, Bochkarev V, McBride CL, Kinney S, Oleynikov D. The patterns and costs of the Da Vinci robotic surgery system in a large academic institution. J Robot Surg. 2008 May;2(1):17-20.
https://doi.org/10.1007/s11701-008-0075-9
PMid:27637212
Higgins RM, Frelich MJ, Bosler ME, Gould JC. Cost analysis of robotic versus laparoscopic general surgery procedures. Surg Endosc. 2017 Jan;31(1):185-92.
https://doi.org/10.1007/s00464-016-4954-2
PMid:27139704
Wilensky GR. Robotic Surgery: An Example of When Newer Is Not Always Better but Clearly More Expensive: Robotic Surgery. Milbank Q. 2016 Mar;94(1):43-6.
https://doi.org/10.1111/1468-0009.12178
PMid:26994707 PMCid:PMC4941968
BenMessaoud C, Kharrazi H, MacDorman KF. Facilitators and Barriers to Adopting Robotic-Assisted Surgery: Contextualizing the Unified Theory of Acceptance and Use of Technology. PLOS ONE. 2011 Jan 20;6(1):e16395.
https://doi.org/10.1371/journal.pone.0016395
PMid:21283719 PMCid:PMC3024425
Kaya Bicer E, Fangerau H, Sur H. Artifical intelligence use in orthopedics: an ethical point of view. EFORT Open Rev. 2023 Aug 1;8(8):592-6.
https://doi.org/10.1530/EOR-23-0083
PMid:37526254 PMCid:PMC10441251
Naik N, Hameed BMZ, Shetty DK, Swain D, Shah M, Paul R, et al. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility? Front Surg. 2022 Mar 14;9:862322.
https://doi.org/10.3389/fsurg.2022.862322
PMid:35360424 PMCid:PMC8963864
Murdoch B. Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Med Ethics. 2021 Dec;22(1):122.
https://doi.org/10.1186/s12910-021-00687-3
PMid:34525993 PMCid:PMC8442400
Jeyaraman M, Balaji S, Jeyaraman N, Yadav S. Unraveling the ethical enigma: artificial intelligence in healthcare. Cureus. 2023 Aug;15(8).
https://doi.org/10.7759/cureus.43262
Tat, Emily, and Mark Rabbat. "Ethical and legal challenges." Machine Learning in Cardiovascular Medicine. Academic Press, 2021. 395-410.
https://doi.org/10.1016/B978-0-12-820273-9.00017-8
Cobianchi L, Verde JM, Loftus TJ, Piccolo D, Dal Mas F, Mascagni P, et al. Artificial Intelligence and Surgery: Ethical Dilemmas and Open Issues. J Am Coll Surg. 2022 Aug;235(2):268-75.
https://doi.org/10.1097/XCS.0000000000000242
PMid:35839401
Soomro NA, Hashimoto DA, Porteous AJ, Ridley CJA, Marsh WJ, Ditto R, et al. Systematic review of learning curves in robot-assisted surgery. BJS Open. 2020 Feb 1;4(1):27-44.
https://doi.org/10.1002/bjs5.50235
PMid:32011823 PMCid:PMC6996634
Chen IHA, Ghazi A, Sridhar A, Stoyanov D, Slack M, Kelly JD, et al. Evolving robotic surgery training and improving patient safety, with the integration of novel technologies. World J Urol. 2021 Aug;39(8):2883-93.
https://doi.org/10.1007/s00345-020-03467-7
PMid:33156361 PMCid:PMC8405494
Fuchs HF, Müller DT, Leers JM, Schröder W, Bruns CJ. Modular step-up approach to robot-assisted transthoracic esophagectomy-experience of a German high volume center. Transl Gastroenterol Hepatol. 2019 Aug;4:62-62.
https://doi.org/10.21037/tgh.2019.07.04
PMid:31559343 PMCid:PMC6737436
Ghaednia H, Fourman MS, Lans A, Detels K, Dijkstra H, Lloyd S, et al. Augmented and virtual reality in spine surgery, current applications and future potentials. Spine J. 2021 Oct;21(10):1617-25.
https://doi.org/10.1016/j.spinee.2021.03.018
PMid:33774210
Andras I, Mazzone E, Van Leeuwen FWB, De Naeyer G, Van Oosterom MN, Beato S, et al. Artificial intelligence and robotics: a combination that is changing the operating room. World J Urol. 2020 Oct;38(10):2359-66.
https://doi.org/10.1007/s00345-019-03037-6
PMid:31776737
Verhelst PJ, Smolders A, Beznik T, Meewis J, Vandemeulebroucke A, Shaheen E, et al. Layered deep learning for automatic mandibular segmentation in cone-beam computed tomography. J Dent. 2021 Nov;114:103786.
https://doi.org/10.1016/j.jdent.2021.103786
PMid:34425172
Shinkawa H, Ishizawa T. Artificial intelligence-based technology for enhancing the quality of simulation, navigation, and outcome prediction for hepatectomy. Artif Intell Surg. 2023;3(1):69-79.
https://doi.org/10.20517/ais.2022.37
Egert M, Steward JE, Sundaram CP. Machine Learning and Artificial Intelligence in Surgical Fields. Indian J Surg Oncol. 2020 Dec;11(4):573-7.
https://doi.org/10.1007/s13193-020-01166-8
PMid:33299275 PMCid:PMC7714893
Park J, Park CH. Recognition and Prediction of Surgical Actions Based on Online Robotic Tool Detection. IEEE Robot Autom Lett. 2021 Apr;6(2):2365-72.
https://doi.org/10.1109/LRA.2021.3060410
Jo YJ, Choi JS, Kim J, Kim HJ, Moon SY. Virtual Reality (VR) Simulation and Augmented Reality (AR) Navigation in Orthognathic Surgery: A Case Report. Appl Sci. 2021 Jun 18;11(12):5673.
https://doi.org/10.3390/app11125673
Kim SH, Lee SJ, Choi MH, Yang HJ, Kim JE, Huh KH, et al. Quantitative Augmented Reality-Assisted Free-Hand Orthognathic Surgery Using Electromagnetic Tracking and Skin-Attached Dynamic Reference. J Craniofac Surg. 2020 Nov;31(8):2175-81.
https://doi.org/10.1097/SCS.0000000000006739
PMid:33136850
Iqbal H, Tatti F, Rodriguez Y Baena F. Augmented reality in robotic assisted orthopaedic surgery: A pilot study. J Biomed Inform. 2021 Aug;120:103841.
https://doi.org/10.1016/j.jbi.2021.103841
PMid:34146717
Omisore OM, Han S, Xiong J, Li H, Li Z, Wang L. A Review on Flexible Robotic Systems for Minimally Invasive Surgery. IEEE Trans Syst Man Cybern Syst. 2022 Jan;52(1):631-44.
https://doi.org/10.1109/TSMC.2020.3026174
Zhu J, Lyu L, Xu Y, Liang H, Zhang X, Ding H, et al. Intelligent Soft Surgical Robots for Next‐Generation Minimally Invasive Surgery. Adv Intell Syst. 2021 May;3(5):2100011.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







