Long Term Ortho-surgical Management of Temporomandibular Joint Ankylosis Secondary to Childhood Infection
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3675Keywords:
Distraction Osteogenesis; Infection; Orthognathic Surgery; Temporomandibular Joint AnkylosisAbstract
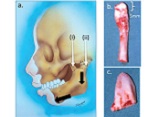
This case report presents the management of a patient suffering from severe facial asymmetry and malocclusion. The patient was born in 2001 and was later hospitalized due to severe jaundice. At 5 years of age, the deviation in the jaws and the post condylectomy ankylosis of the TMJ and hip joint problems were evident. At age 7, a costochondral graft was performed. In the next phase, orthodontic treatment was started with hybrid functional therapy, but the treatment was unsuccessful due to the severity of the problem. At age 15, bilateral distraction osteogenesis was performed. The orthodontic plan for the maxilla was non-extraction. We expanded the upper arch and corrected the crossbite of the lateral incisors. Due to the difficulty of surgery, the impacted canine of the mandible remained impacted. The mandibular right lower incisor was removed due to severe crowding. Orthognathic surgery was performed after fixed orthodontic treatment.
References
Mittal N, Goyal M, Sardana D, Dua JS. Outcomes of surgical management of TMJ ankylosis: A systematic review and meta-analysis. J Craniomaxillofac Surg. 2019;47(7):1120-33.
https://doi.org/10.1016/j.jcms.2019.03.029
PMid:31027859
Ramly EP, Yu JW, Eisemann BS, Yue O, Alfonso AR, Kantar RS, et al. Temporomandibular Joint Ankylosis in Pediatric Patients With Craniofacial Differences: Causes, Recurrence and Clinical Outcomes. J Craniofac Surg. 2020;31(5):1343-7.
https://doi.org/10.1097/SCS.0000000000006328
PMid:32176014
Al-Moraissi EA, El-Sharkawy TM, Mounair RM, El-Ghareeb TI. A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2015;44(4):470-82.
https://doi.org/10.1016/j.ijom.2014.10.017
PMid:25468632
Topazian RG. Infectious arthritis of the temporomandibular joint. Oral and maxillofacial infections. Saunders, Philadelphia. 1987:336-7.
Chaves Netto HD, Nascimento FF, Chaves M, Chaves LM, Negreiros Lyrio MC, Mazzonetto R. TMJ ankylosis after neonatal septic arthritis: literature review and two case reports. Oral Maxillofac Surg. 2011;15(2):113-9.
https://doi.org/10.1007/s10006-010-0210-4
PMid:20369268
Alexander WN, Nagy WW. Gonococcal arthritis of the temporomandibular joint. Report of a case. Oral Surg Oral Med Oral Pathol. 1973;36(6):809-13.
https://doi.org/10.1016/0030-4220(73)90331-9
PMid:4524832
Kasznia-Kocot J, Cichos B, Sada-Cieślar M, Buszman Z. [Staphylococcal septicemia in a newborn infant with multiple organ involvement]. Wiad Lek. 1990;43(7):301-4.
Shetty V, Kishore PN, Khanum A, Yadav A, Sailer HF. Retrospective analysis of a TMJ ankylosis protocol with a 9 year follow up. Journal of Cranio-Maxillofacial Surgery. 2019 Dec 1;47(12):1903-12.
https://doi.org/10.1016/j.jcms.2019.11.003
PMid:31812309
Jiang Y, Huang Y, Ye B, Li Y, Zhu S. Management of Temporomandibular Joint Ankylosis With Dentofacial Deformities in Children. J Craniofac Surg. 2018;29(2):e150-e5.
https://doi.org/10.1097/SCS.0000000000004253
PMid:29381640
Das UM, Keerthi R, Ashwin DP, VenkataSubramanian R, Reddy D, Shiggaon N. Ankylosis of temporomandibular joint in children. J Indian Soc Pedod Prev Dent. 2009;27(2):116-20.
https://doi.org/10.4103/0970-4388.55338
PMid:19736506
Khanna JN, Ramaswami R. Protocol for the management of ankylosis of the temporomandibular joint. Br J Oral Maxillofac Surg. 2019;57(10):1113-8.
https://doi.org/10.1016/j.bjoms.2019.10.298
PMid:31732273
Leighty SM, Spach DH, Myall RW, Burns JL. Septic arthritis of the temporomandibular joint: review of the literature and report of two cases in children. Int J Oral Maxillofac Surg. 1993;22(5):292-7.
https://doi.org/10.1016/S0901-5027(05)80519-3
PMid:8245570
Regev E, Koplewitz BZ, Nitzan DW, Bar-Ziv J. Ankylosis of the temporomandibular joint as a sequela of septic arthritis and neonatal sepsis. Pediatr Infect Dis J. 2003;22(1):99-101.
https://doi.org/10.1097/00006454-200301000-00028
PMid:12553307
Güven O, Keskin A. Remodelling following condylar fractures in children. Journal of Cranio-Maxillofacial Surgery. 2001 Aug 1;29(4):232-7.
https://doi.org/10.1054/jcms.2001.0228
PMid:11562093
Bounds GA, Hopkins R, Sugar A. Septic arthritis of the temporo-mandibular joint--a problematic diagnosis. Br J Oral Maxillofac Surg. 1987;25(1):61-7.
https://doi.org/10.1016/0266-4356(87)90158-6
PMid:2948546
O'Meara PM, Bartal E. Septic arthritis: process, etiology, treatment outcome. A literature review. Orthopedics. 1988;11(4):623-8.
https://doi.org/10.3928/0147-7447-19880401-14
PMid:3290872
Parmar J. Case Report: septic arthritis of the temporomandibular joint in a neonate. Br J Oral Maxillofac Surg. 2008;46(6):505-6.
https://doi.org/10.1016/j.bjoms.2008.01.005
PMid:18282642
Hincapie JW, Tobon D, Diaz-Reyes GA. Septic arthritis of the temporomandibular joint. Otolaryngology- Head Neck Surgery. 1999;121(6):836-7.
https://doi.org/10.1053/hn.1999.v121.a96115
PMid:10580251
Sllamniku S, Raka L, Haxhija EQ, Murtezani A. Hip Ankylosis after Untreated Septic Arthritis by Escherichia coli: A Case Report. Revista Brasileira de Ortopedia. 2024 Sep 30;59:22-5.
https://doi.org/10.1055/s-0041-1736515
PMid:39027173 PMCid:PMC11254424
Goldschmidt MJ, Butterfield KJ, Goracy ES, Goldberg MH. Streptococcal infection of the temporomandibular joint of hematogenous origin: a case report and contemporary therapy. J Oral Maxillofac Surg. 2002;60(11):1347-53.
https://doi.org/10.1053/joms.2002.35736
PMid:12420272
Lazzarotto A, Tel A, Nocini R, Raccampo L, Sembronio S, Costa F, et al. Custom-made alloplastic prosthetic implant to treat temporomandibular joint ankylosis in pediatric patients: A case study. Applied Sciences. 2021;12(1):142.
https://doi.org/10.3390/app12010142
Cho JW, Park JH, Kim JW, Kim SJ. The sequential management of recurrent temporomandibular joint ankylosis in a growing child: a case report. Maxillofac Plast Reconstr Surg. 2016;38(1):39.
https://doi.org/10.1186/s40902-016-0083-z
PMid:27774442 PMCid:PMC5050230
Valentini V, Califano L, Cassoni A, Marco DM, Raponi I, Priore P, et al. Maxillo-Mandibular Reconstruction in Pediatric Patients: How To Do It? J Craniofac Surg. 2018;29(3):761-6.
https://doi.org/10.1097/SCS.0000000000004380
PMid:29438212
Awal DH, Jaffer M, Charan G, Ball RE, Kennedy G, Thomas S, et al. Costochondral grafting for paediatric temporomandibular joint reconstruction: 10-year outcomes in 55 cases. Int J Oral Maxillofac Surg. 2018;47(11):1433-8.
https://doi.org/10.1016/j.ijom.2018.06.004
PMid:29960838
Ko EW, Huang CS, Chen YR. Temporomandibular joint reconstruction in children using costochondral grafts. Journal of oral and maxillofacial surgery. 1999 Jul 1;57(7):789-98.
https://doi.org/10.1016/S0278-2391(99)90816-9
PMid:10416625
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







