Managing Local Bleeding in Dentoalveolar Surgery: Practical Techniques and Best Practices: A Narrative Review
DOI:
https://doi.org/10.31661/gmj.v13iSP1.3686Keywords:
Dentoalveolar Surgery; Hemostasis; Surgical Hemorrhage Control Anticoagulants; Hemostatic AgentsAbstract
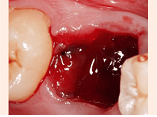
Effective management of local bleeding is essential for safe and successful dentoalveolar surgery, particularly among patients with bleeding disorders, those on anticoagulant therapy, or individuals with systemic conditions affecting hemostasis. This narrative review explores practical and advanced approaches for controlling bleeding in dentoalveolar procedures, with a focus on patient-centered strategies that minimize risk while accommodating complex clinical needs. Based on this narriative review, Beginning with an overview of the pathophysiology of bleeding in the oral cavity, the review examines conventional methods such as mechanical compression, sutures, and the use of local anesthetics with vasoconstrictors. Further, it evaluates the application of pharmacological agents, including topical hemostatic products like gelatin sponges, oxidized cellulose, and tranexamic acid, which have shown efficacy in high-risk patients without disrupting systemic anticoagulation therapy. For special populations, including those with congenital coagulopathies and liver disease, tailored approaches are reviewed to address unique bleeding challenges. Additionally, innovative hemostatic materials and laser-assisted techniques are discussed as emerging options that promise enhanced safety and effectiveness in complex cases. By synthesizing current knowledge on bleeding control methods, this review provides clinicians with practical guidance for optimizing hemostasis in dentoalveolar surgery. The insights and recommendations presented aim to improve patient outcomes, reduce perioperative complications, and support a balanced approach to local and systemic hemostatic management in diverse patient groups.
References
Broekema FI, van Minnen B, Jansma J, Bos RR. Risk of bleeding after dentoalveolar surgery in patients taking anticoagulants. British Journal of Oral and Maxillofacial Surgery. 2014;52(3):e15-e9.
https://doi.org/10.1016/j.bjoms.2014.01.006
PMid:24485810
Rech B, Tenório J, Franco J, Medina J, Gallottini M, Pérez‐Sayáns M, Ortega K. Risk of bleeding during oral surgery in patients with liver cirrhosis: A systematic review. Journal of the American Dental Association. 2021;152(1):46-54.
https://doi.org/10.1016/j.adaj.2020.09.018
PMid:33250169
van Dijk WE, van Es RJ, Correa ME, Schutgens RE, van Galen KP. Dentoalveolar procedures in immune thrombocytopenia; systematic review and an institutional guideline. TH Open. 2021;5(04):e489-e502.
https://doi.org/10.1055/a-1641-7770
PMid:34805736 PMCid:PMC8595053
Miziara LNB, Sendyk WR, Ortega KL, Gallottini M, Sendyk DI, Martins F, et al. Risk of bleeding during implant surgery in patients taking antithrombotics: a systematic review. Seminars in Thrombosis and Hemostasis. 2021;47(6):702-708.
https://doi.org/10.1055/s-0041-1722845
PMid:33971681
Cetira Filho EL, Franco JMPL, Ribeiro TR, de Barros Silva PG, Costa FWG. Does platelet-rich fibrin prevent hemorrhagic complications after dental extractions in patients using oral anticoagulant therapy? Journal of Oral and Maxillofacial Surgery. 2021;79(11):2215-26.
https://doi.org/10.1016/j.joms.2021.07.003
PMid:34343502
Dawoud BE, Kent S, Tabbenor O, George P, Dhanda J. Dental implants and risk of bleeding in patients on oral anticoagulants: a systematic review and meta-analysis. International Journal of Implant Dentistry. 2021;7:1-8.
https://doi.org/10.1186/s40729-021-00364-5
PMid:34430994 PMCid:PMC8385035
AlSheef M, Gray J, AlShammari A. Risk of postoperative bleeding following dental extractions in patients on antithrombotic treatment. The Saudi Dental Journal. 2021;33(7):511-7.
https://doi.org/10.1016/j.sdentj.2020.09.005
PMid:34803294 PMCid:PMC8589605
Bajkin BV, Wahl MJ, Miller CS. Dental implant surgery and risk of bleeding in patients on antithrombotic medications: A review of the literature. Oral surgery, oral medicine, oral pathology and oral radiology. 2020;130(5):522-32.
https://doi.org/10.1016/j.oooo.2020.07.012
PMid:32811791
Federici a, Sacco a, Stabile a, Carpenedo a, Zingaro a, Mannucci a. Optimising local therapy during oral surgery in patients with von Willebrand disease: effective results from a retrospective analysis of 63 cases. Haemophilia. 2000;6(2):71-7.
https://doi.org/10.1046/j.1365-2516.2000.00370.x
PMid:10781191
Ward BB, Weideman EM. Long-term postoperative bleeding after dentoalveolar surgery in the pretransplant liver failure patient. Journal of oral and maxillofacial surgery. 2006;64(10):1469-74.
https://doi.org/10.1016/j.joms.2006.05.044
PMid:16982303
Katsumi Y, Tanaka R, Hayashi T, Koga T, Takagi R, Ohshima H. Variation in arterial supply to the floor of the mouth and assessment of relative hemorrhage risk in implant surgery. Clinical Oral Implants Research. 2013;24(4):434-40.
https://doi.org/10.1111/j.1600-0501.2011.02348.x
PMid:22092873
Czembirek C, Poeschl WP, Eder-Czembirek C, Fischer MB, Perisanidis C, Jesch P et al. Causes and timing of delayed bleeding after oral surgery. Clinical oral investigations. 2014;18:1655-61.
https://doi.org/10.1007/s00784-013-1133-x
PMid:24287889
Jensen PS. Hemorrhage after oral surgery: an analysis of 103 cases. Oral Surgery, Oral Medicine, Oral Pathology. 1974;37(1):2-16.
https://doi.org/10.1016/0030-4220(74)90154-6
PMid:4543442
Lozano A, Pérez M, Esteve C. Dental management in patients with hemostasis alteration. Journal of Clinical and Experimental Dentistry. 2011;3:120-6. doi:10.4317/JCED.3.E120.
https://doi.org/10.4317/jced.3.e120
Reich W, Kriwalsky MS, Wolf HH, Schubert J. Bleeding complications after oral surgery in outpatients with compromised haemostasis: incidence and management. Oral and maxillofacial surgery. 2009;13:73-7.
https://doi.org/10.1007/s10006-009-0154-8
PMid:19319581
Israels S, Schwetz N, Boyar R, McNicol A. Bleeding disorders: characterization, dental considerations and management. Journal of the Canadian Dental Association. 2006;72(9):827.
Partridge CG, Campbell J. The effect of platelet-altering medications on bleeding from minor oral surgery. Journal of Oral and Maxillofacial Surgery. 2004;62:33.
https://doi.org/10.1016/j.joms.2004.05.161
van Galen KP, Engelen ET, Mauser‐Bunschoten EP, van Es RJ, Schutgens RE. Antifibrinolytic therapy for preventing oral bleeding in patients with haemophilia or Von Willebrand disease undergoing minor oral surgery or dental extractions. Cochrane Database of Systematic Reviews. 2019; (4): CD011385.
https://doi.org/10.1002/14651858.CD011385.pub3
PMid:31002742 PMCid:PMC6474399
Bajkin BV, Popovic SL, Selakovic SD. Randomized, prospective trial comparing bridging therapy using low-molecular-weight heparin with maintenance of oral anticoagulation during extraction of teeth. Journal of oral and maxillofacial surgery. 2009;67(5):990-5.
https://doi.org/10.1016/j.joms.2008.12.027
PMid:19375008
Pulicari F, Pellegrini M, Scribante A, Kuhn E, Spadari F. Pathological Background and Clinical Procedures in Oral Surgery Haemostasis Disorders: A Narrative Review. Applied Sciences. 2023;13(4):2076.
https://doi.org/10.3390/app13042076
Mp SK. Local hemostatic agents in the management of bleeding in oral surgery. Asian J Pharm Clin Res. 2016;9(3):35-41.
Campos FHdO, Ferreira LB, Romano MM, Moreira MS, Eduardo CdP, Ramalho KM. Immediate laser-induced hemostasis in anticoagulated rats subjected to oral soft tissue surgery: a double-blind study. Brazilian Oral Research. 2018;32:e56.
https://doi.org/10.1590/1807-3107bor-2018.vol32.0056
Rapaport SI. Preoperative hemostatic evaluation: which tests, if any? Blood. 1983;61(2):229-31.
https://doi.org/10.1182/blood.V61.2.229.229
PMid:6821695
Lizbeth DVT, Oscar CM. Preoperative Bleeding Risk Assessment. International Journal of Medical Science and Clinical Research Studies. 2023;3(05):940-2.
Helenius-Hietala J, Åberg F, Meurman JH, Nordin A, Isoniemi H. Oral surgery in liver transplant candidates: a retrospective study on delayed bleeding and other complications. Oral surgery, oral medicine, oral pathology and oral radiology. 2016;121(5):490-5.
https://doi.org/10.1016/j.oooo.2016.01.025
PMid:27068309
Bajkin BV, Vujkov SB, Milekic BR, Vuckovic BA. Risk factors for bleeding after oral surgery in patients who continued using oral anticoagulant therapy. The Journal of the American Dental Association. 2015;146(6):375-81.
https://doi.org/10.1016/j.adaj.2015.01.017
PMid:26025824
Wilson RD. Preoperative diagnosis and management of inherited bleeding disorders in female adolescents and adults. Canadian Journal of Surgery. 2023;66(3):E246.
https://doi.org/10.1503/cjs.005922
PMid:37130707 PMCid:PMC10158752
Cosmi B, Alatri A, Cattaneo M, Gresele P, Marietta M, Rodeghiero F et al. Assessment of the risk of bleeding in patients undergoing surgery or invasive procedures: Guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thrombosis research. 2009;124(5):e6-e12.
https://doi.org/10.1016/j.thromres.2009.08.005
PMid:19740528
Cohn SL. Preoperative Evaluation for Noncardiac Surgery (Japanese Version). Annals of internal medicine. 2016;165(11):JITC81-JITC96.
https://doi.org/10.7326/IsTranslatedFrom_AITC201612060_Japanese
PMid:30140906
Charlton NP, Solberg R, Rizer J, Singletary E, Woods WA. Pressure methods for primary hemorrhage control: a randomized crossover trial. International Journal of First Aid Education. 2019;2(1):19-27.
https://doi.org/10.21038/ijfa.2018.0011
Kale TP, Singh AK, Kotrashetti S, Kapoor A. Effectiveness of Hemcon dental dressing versus conventional method of haemostasis in 40 patients on oral antiplatelet drugs. Sultan Qaboos University Medical Journal. 2012;12(3):330.
https://doi.org/10.12816/0003147
PMid:22912926 PMCid:PMC3413624
Naimer SA, Chemla F. Elastic adhesive dressing treatment of bleeding wounds in trauma victims. The American journal of emergency medicine. 2000;18(7):816-9.
https://doi.org/10.1053/ajem.2000.18126
PMid:11103736
Scott-Conner CE, Chassin JL. Control of Bleeding. Chassin's Operative Strategy in General Surgery: An Expositive Atlas Springer; 2013.
https://doi.org/10.1007/978-1-4614-1393-6_6
Dutta S, Mukherjee A, Saha J, Biswas G, Haldar D, Sen I, Sinha R. Modified technique of anterior nasal packing: a comparative study report. Indian Journal of Otolaryngology and Head & Neck Surgery. 2012;64:341-5.
https://doi.org/10.1007/s12070-011-0343-2
PMid:24294575 PMCid:PMC3477445
Naimer SA, Anat N, Katif G, Team R. Evaluation of techniques for treating the bleeding wound. Injury. 2004;35(10):974-9.
https://doi.org/10.1016/S0020-1383(03)00316-4
PMid:15351660
McKee JL, Kirkpatrick AW, Bennett BL, Jenkins DA, Logsetty S, Holcomb JB. Worldwide Case Reports Using the iTClamp for External Hemorrhage Control. Journal of special operations medicine: a peer reviewed journal for SOF medical professionals. 2018;18(3):39-44.
https://doi.org/10.55460/ZIY0-8LIH
PMid:30222835
John AES, Wang X, Lim EB, Chien D, Stern SA, White NJ. Effects of rapid wound sealing on survival and blood loss in a swine model of lethal junctional arterial hemorrhage. Journal of Trauma and Acute Care Surgery. 2015;79(2):256-62.
https://doi.org/10.1097/TA.0000000000000746
PMid:26218694
Studdiford W. Absorbable (oxidized) gauze as a hemostatic agent in gynecologic surgery. American Journal of Obstetrics and Gynecology. 1946;52(3):495-9.
https://doi.org/10.1016/S0002-9378(15)30269-6
PMid:20998170
Hvas A-M, Larsen JB, Pasalic L, et al. Thrombosis and hemostasis in surgery. Seminars in Thrombosis and Hemostasis: Thieme Medical Publishers ; 2017.
https://doi.org/10.1055/s-0037-1605571
PMid:28962042
Chiarantini E, Valanzano R, Liotta AA, Cellai AP, Ilari I, Prisco D et al. Persistence of hemostatic alterations in patients affected by Crohn's disease after bowel surgery. Thrombosis research. 1997;87(6):539-46.
https://doi.org/10.1016/S0049-3848(97)00183-7
PMid:9330436
Manoj Agarwal M, Sankalp Mittal M, Sharmistha Vijay M, Pooja Yadav M, Panwar VR, Gupta N. Management of the Dental Patient on Anticogulant Medication. The New York state dental journal. 2014; 80(4):29-32.
Nuvvula S, Gaddam KR, Kamatham R. Efficacy of tranexamic acid mouthwash as an alternative for factor replacement in gingival bleeding during dental scaling in cases of hemophilia: a randomized clinical trial. Contemporary clinical dentistry. 2014;5(1):49-53.
https://doi.org/10.4103/0976-237X.128663
PMid:24808695 PMCid:PMC4012117
Ambrogio RI, Levine MH. Tranexamic acid as a hemostatic adjunct in dentistry. Compendium. 2018;39(6):392-401.
Muskett A, W Henry Barber V, Lineaweaver WC. The plastic surgeon's guide to drugs affecting hemostasis. Annals of plastic surgery. 2005;54(5):570-6.
https://doi.org/10.1097/01.sap.0000157893.66050.98
PMid:15838223
Erstad BL. What is the evidence for using hemostatic agents in surgery? Haemostasis in Spine Surgery. 2005:28-33.
https://doi.org/10.1007/3-540-27394-8_5
Malmquist JP, Clemens SC, Oien HJ, Wilson SL. Hemostasis of oral surgery wounds with the HemCon Dental Dressing. Journal of Oral and Maxillofacial Surgery. 2008;66(6):1177-83.
https://doi.org/10.1016/j.joms.2007.12.023
PMid:18486782
Levett DZ, Edwards M, Grocott M, Mythen M. Preparing the patient for surgery to improve outcomes. Best practice & research Clinical anaesthesiology. 2016;30(2):145-57.
https://doi.org/10.1016/j.bpa.2016.04.002
PMid:27396803
Burch J, Balfour A. Preoperative patient education. Enhanced Recovery After Surgery: A Complete Guide to Optimizing Outcomes. 2020:37-49.
https://doi.org/10.1007/978-3-030-33443-7_5
Zhu H, Zhang L, Cai Z, Shan X. Dental Implant Rehabilitation After Jaw Reconstruction Assisted by Virtual Surgical Planning. International Journal of Oral & Maxillofacial Implants. 2019;34(5):1223.
https://doi.org/10.11607/jomi.7278
PMid:30892283
Kalbfell E, Kata A, Buffington AS, Marka N, Brasel KJ, Mosenthal AC et al. Frequency of preoperative advance care planning for older adults undergoing high-risk surgery: a secondary analysis of a randomized clinical trial. JAMA surgery. 2021;156(7):e211521-e.
https://doi.org/10.1001/jamasurg.2021.1521
PMid:33978693 PMCid:PMC8117055
Slezak P, Keibl C, Labahn D, Schmidbauer A, Genyk Y, Gulle H. A comparative efficacy evaluation of recombinant topical thrombin (RECOTHROM®) with a gelatin sponge carrier versus topical oxidized regenerated cellulose (TABOTAMP®/SURGICEL®) in a porcine liver bleeding model. Journal of Investigative Surgery. 2021;34(8):862-8.
https://doi.org/10.1080/08941939.2019.1705444
PMid:31955627
Li S, Wu X, Bai N, Ni J, Liu X, Mao W et al. Fabricating oxidized cellulose sponge for hemorrhage control and wound healing. ACS Biomaterials Science & Engineering. 2023;9(11):6398-408.
https://doi.org/10.1021/acsbiomaterials.3c00018
PMid:37126763
Ibne Mahbub MS, Sultana T, Gwon J-G, Lee B-T. Fabrication of thrombin loaded TEMPO-oxidized cellulose nanofiber-gelatin sponges and their hemostatic behavior in rat liver hemorrhage model. Journal of Biomaterials Science, Polymer Edition. 2022;33(4):499-516.
https://doi.org/10.1080/09205063.2021.1992877
PMid:34644247
Khanna P, Mahajan C, Gupta P, Banik S, Ray BR, Rath GP. Use of gelatin-thrombin matrix haemostatic sealant in neurosurgery: Anaesthetic implications and review of literature. Journal of Neuroanaesthesiology and Critical Care. 2015;2(01):051-4.
https://doi.org/10.4103/2348-0548.148391
Ranjbar J, Koosha M, Chi H, Ghasemi A, Zare F, Abdollahifar MA et al. Novel chitosan/gelatin/oxidized cellulose sponges as absorbable hemostatic agents. Cellulose. 2021;28:3663-75.
https://doi.org/10.1007/s10570-021-03699-9
Takagi T, Tsujimoto H, Torii H, Ozamoto Y, Hagiwara A. Two-layer sheet of gelatin: A new topical hemostatic agent. Asian journal of surgery. 2018;41(2):124-30.
https://doi.org/10.1016/j.asjsur.2016.09.007
PMid:27816406
Bochicchio GV, Gupta N, Porte RJ, Renkens KL, Pattyn P, Topal B et al. The FINISH-3 trial: a phase 3, international, randomized, single-blind, controlled trial of topical fibrocaps in intraoperative surgical hemostasis. Journal of the American College of Surgeons. 2015;220(1):70-81.
https://doi.org/10.1016/j.jamcollsurg.2014.09.019
PMid:25458801
Prabhu S, Prabhu S. Bespoke gelfoam wafers: A practical and inexpensive alternative to oxycel for hemostasis during neurosurgery. Asian journal of neurosurgery. 2019;14(02):483-6.
https://doi.org/10.4103/ajns.AJNS_275_18
PMid:31143266 PMCid:PMC6516018
Ockerman A, Vanhaverbeke M, Miclotte I, Belmans A, Vanassche T, Politis C, Jacobs R, Verhamme P. Tranexamic acid to reduce bleeding after dental extraction in patients treated with non-vitamin K oral anticoagulants: design and rationale of the EXTRACT-NOAC trial. British Journal of Oral and Maxillofacial Surgery. 2019 Dec 1;57(10):1107-12.
https://doi.org/10.1016/j.bjoms.2019.10.297
PMid:31669068
de Vasconcellos SJdA, de Santana Santos T, Reinheimer DM, Faria-e-Silva AL, de Melo MdFB, Martins-Filho PRS. Topical application of tranexamic acid in anticoagulated patients undergoing minor oral surgery: A systematic review and meta-analysis of randomized clinical trials. Journal of Cranio-Maxillofacial Surgery. 2017;45(1):20-6.
https://doi.org/10.1016/j.jcms.2016.10.001
PMid:27840121
Soares ECS, Costa FWG, Bezerra TP, Nogueira CBP, de Barros Silva PG, Batista SHB et al. Postoperative hemostatic efficacy of gauze soaked in tranexamic acid, fibrin sponge, and dry gauze compression following dental extractions in anticoagulated patients with cardiovascular disease: a prospective, randomized study. Oral and maxillofacial surgery. 2015;19:209-16.
https://doi.org/10.1007/s10006-014-0479-9
PMid:25528251
Queiroz SIML, Silvestre VD, Soares RM, Campos GBP, Germano AR, da Silva JSP. Tranexamic acid as a local hemostasis method after dental extraction in patients on warfarin: a randomized controlled clinical study. Clinical oral investigations. 2018;22:2281-9.
https://doi.org/10.1007/s00784-017-2327-4
PMid:29374327
Pippi R, Santoro M, Cafolla A. The use of a chitosan-derived hemostatic agent for postextraction bleeding control in patients on antiplatelet treatment. Journal of Oral and Maxillofacial Surgery. 2017;75(6):1118-23.
https://doi.org/10.1016/j.joms.2017.01.005
PMid:28189659
Beverly A, Ong G, Kimber C, Sandercock J, Doree C, Welton NJ et al. Drugs to reduce bleeding and transfusion in major open vascular or endovascular surgery: a systematic review and network meta‐analysis. Cochrane Database of Systematic Reviews. 2023; (2):CD013649.
https://doi.org/10.1002/14651858.CD013649.pub2
PMid:36800489 PMCid:PMC9936832
Genyk Y, Kato T, Pomposelli JJ, Wright Jr KJ, Sher LS, Tetens V, Chapman WC. Fibrin sealant patch (TachoSil) vs oxidized regenerated cellulose patch (Surgicel Original) for the secondary treatment of local bleeding in patients undergoing hepatic resection: a randomized controlled trial. Journal of the American College of Surgeons. 2016;222(3):261-8.
https://doi.org/10.1016/j.jamcollsurg.2015.12.007
PMid:26776356
Gazzeri R, Galarza M, Fiore C, Callovini G, Alfieri A. Use of tissue-glue-coated collagen sponge (TachoSil) to repair minor cerebral dural venous sinus lacerations. Operative Neurosurgery. 2015;11(1):32-6.
https://doi.org/10.1227/NEU.0000000000000614
PMid:25584959
Zheng C, Liu X, Luo X, Zheng M, Wang X, Dan W, Jiang H. Development of a novel bio-inspired "cotton-like" collagen aggregate/chitin based biomaterial with a biomimetic 3D microstructure for efficient hemostasis and tissue repair. Journal of Materials Chemistry B. 2019;7(46):7338-50.
https://doi.org/10.1039/C9TB02028D
PMid:31693046
Ramot Y, Steiner M, Lavie Y, Ezov N, Laub O, Cohen E et al. Safety and efficacy of sFilm-FS, a novel biodegradable fibrin sealant, in Göttingen minipigs. Journal of toxicologic pathology. 2021;34(4):319-30.
https://doi.org/10.1293/tox.2021-0030
PMid:34629733 PMCid:PMC8484930
Malik AK, Amer AO, Tingle SJ, Thompson ER, White SA, Manas DM, Wilson C. Fibrin‐based haemostatic agents for reducing blood loss in adult liver resection. Cochrane Database of Systematic Reviews. 2023;(8):CD010872.
https://doi.org/10.1002/14651858.CD010872.pub2
PMid:37551841 PMCid:PMC10411946
Kobayashi S, Takeda Y, Nakahira S, Tsujie M, Shimizu J, Miyamoto A et al. Fibrin sealant with polyglycolic acid felt vs fibrinogen-based collagen fleece at the liver cut surface for prevention of postoperative bile leakage and hemorrhage: a prospective, randomized, controlled study. Journal of the American College of Surgeons. 2016;222(1):59-64.
https://doi.org/10.1016/j.jamcollsurg.2015.10.006
PMid:26597705
Long M, Zhang Y, Huang P, Chang S, Hu Y, Yang Q et al. Emerging nanoclay composite for effective hemostasis. Advanced Functional Materials. 2018;28(10):1704452.
https://doi.org/10.1002/adfm.201704452
Gheorghiță D, Moldovan H, Robu A, Bița A-I, Grosu E, Antoniac A et al. Chitosan-Based Biomaterials for Hemostatic Applications: A Review of Recent Advances. International journal of molecular sciences. 2023;24(13):10540.
https://doi.org/10.3390/ijms241310540
PMid:37445718 PMCid:PMC10342007
Yang Z, Chen L, Liu J, Zhuang H, Lin W, Li C, Zhao X. Short peptide nanofiber biomaterials ameliorate local hemostatic capacity of surgical materials and intraoperative hemostatic applications in clinics. Advanced Materials. 2023;35(39):2301849.
https://doi.org/10.1002/adma.202301849
PMid:36942893
Atashgahi M, Ghaemi B, Valizadeh A, Moshiri A, Nekoofar MH, Amani A. Epinephrine-entrapped chitosan nanoparticles covered by gelatin nanofibers: A bi-layer nano-biomaterial for rapid hemostasis. International Journal of Pharmaceutics. 2021;608:121074.
https://doi.org/10.1016/j.ijpharm.2021.121074
PMid:34481888
Cheng J, Liu J, Li M, Liu Z, Wang X, Zhang L, Wang Z. Hydrogel-based biomaterials engineered from natural-derived polysaccharides and proteins for hemostasis and wound healing. Frontiers in Bioengineering and Biotechnology. 2021;9:780187.
https://doi.org/10.3389/fbioe.2021.780187
PMid:34881238 PMCid:PMC8645981
Kozyreva E, Ryabova M. Experimental justification of laser parameters for preventive laser (970 nm) vessel coagulation in intraoperative bleeding. Regional blood circulation and microcirculation. 2018;17(4):57-61.
https://doi.org/10.24884/1682-6655-2018-17-4-57-61
da Silva Grigio G, Tateno RY, Palma LF, Shitsuka C, Sendyk WR, Campos L. High-power diode laser for second-stage implant surgery: a randomized pilot clinical trial. Research, Society and Development. 2020;9(7):e128974122-e.
https://doi.org/10.33448/rsd-v9i7.4122
Larionova EV, Diachkova EY, Morozova EA, Davtyan AA, Tarasenko SV. Laser-assisted tooth extraction in patients with impaired hemostasis. Biomedicine. 2021;11(2):47.
https://doi.org/10.37796/2211-8039.1072
PMid:35223404 PMCid:PMC8824248
Suter V, Altermatt H, Bornstein M. A randomized controlled trial comparing surgical excisional biopsies using CO2 laser, Er: YAG laser and scalpel. International journal of oral and maxillofacial surgery. 2020;49(1):99-106.
https://doi.org/10.1016/j.ijom.2019.05.012
PMid:31230766
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







