Effects of Dimethyl Fumarate on the Karnofsky Performance Status and Serum S100β Level in Newly Glioblastoma Patients: A Randomized, Phase-II, Placebo, Triple Blinded, Controlled Trial
DOI:
https://doi.org/10.31661/gmj.v11i.1897Keywords:
Glioblastoma, Kanofsky's Performance Status, Dimethyl Fumarate, S100β, Surgical Brain InjuryAbstract
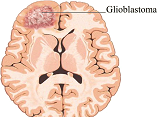
Background: Glioblastoma (GBM) is the most common primary central nervous system malignancy with a low survival without extra logistics. Currently, there is no definitive chemotherapy among the studied options. This study aims to evaluate the neuroprotective effects of dimethyl fumarate (DMF) on surgical brain injuries in patients treated for GBM. Materials and Methods: This randomized, phase II, placebo, triple-blinded, controlled trial was performed on 36 patients with a diagnosis of GBM. All the patients received DMF (240 mg, three-times per day) or placebo (with the same shape and administration route) one week before surgery. Also, patients in both groups after the operation received standard treatments (radiotherapy plus chemotherapy). In addition, Kanofsky's performance status (KPS) score was evaluated at baseline and one month later. Also, serum S100β was measured 48 hours before and after surgery. Results: There was no significant difference among DMF and control groups with regard to age, gender, and the extent of resections (P˃0.05). The most adverse event in both groups was a headache. Although the serum S100β level was not markedly changed after surgery, the mean KPS in the DMF group was higher than in the control group after surgery. Conclusion: The DMF could be a possible good regime for the treatment of GBM; however, questions are raised regarding its efficacy and application for the addition to standard treatment.[GMJ.2022;11:e1897]
References
Hosseini MM, Karimi A, Behroozaghdam M, Javidi MA, Ghiasvand S, Bereimipour A, et al. Cytotoxic and Apoptogenic Effects of Cyanidin-3-Glucoside on the Glioblastoma Cell Line. World Neurosurg. 2017;108:94-100. https://doi.org/10.1016/j.wneu.2017.08.133PMid:28867321 Chen B, Chen C, Zhang Y, Xu J. Recent incidence trend of elderly patients with glioblastoma in the United States, 2000-2017. BMC Cancer. 2021;21(1):54. https://doi.org/10.1186/s12885-020-07778-1PMid:33430813 PMCid:PMC7802341 Lu VM, Jue TR, McDonald KL, Rovin RA. The Survival Effect of Repeat Surgery at Glioblastoma Recurrence and its Trend: A Systematic Review and Meta-Analysis. World Neurosurg. 2018;115:453-9.e3. https://doi.org/10.1016/j.wneu.2018.04.016PMid:29654958 Tykocki T, Eltayeb M. Ten-year survival in glioblastoma. A systematic review. J Clin Neurosci. 2018;54:7-13. https://doi.org/10.1016/j.jocn.2018.05.002PMid:29801989 Wen PY, Weller M, Lee EQ, Alexander BM, Barnholtz-Sloan JS, Barthel FP, et al. Glioblastoma in adults: a Society for Neuro-Oncology (SNO) and European Society of Neuro-Oncology (EANO) consensus review on current management and future directions. Neuro Oncol. 2020;22(8):1073-113. https://doi.org/10.1093/neuonc/noaa106PMid:32328653 PMCid:PMC7594557 Raucher D. Tumor targeting peptides: novel therapeutic strategies in glioblastoma. Curr Opin Pharmacol. 2019;47:14-9. https://doi.org/10.1016/j.coph.2019.01.006PMid:30776641 PMCid:PMC7288394 Gramatzki D, Roth P, Rushing EJ, Weller J, Andratschke N, Hofer S, et al. Bevacizumab may improve quality of life, but not overall survival in glioblastoma: an epidemiological study. Ann Oncol. 2018;29(6):1431-6. https://doi.org/10.1093/annonc/mdy106PMid:29617713 Zhao M, van Straten D, Broekman MLD, Préat V, Schiffelers RM. Nanocarrier-based drug combination therapy for glioblastoma. Theranostics. 2020;10(3):1355-72. https://doi.org/10.7150/thno.38147PMid:31938069 PMCid:PMC6956816 Abbasy Z, Arani HZ, Ale-Ebrahim M, Moodi V, Nematian J, Barati M, Shafaie S, Ansari AM, Hashemi A, Davoodi P, Javidi MA. Simultaneous Treatment with P53 Overexpression and Interferon γ Exerts a Dramatic Increase in Apoptosis Induction of U87 Cells. Galen Med J. 2021;10:e2270. https://doi.org/10.31661/gmj.v10i0.2270 Ahmadi-Beni R, Najafi A, Savar SM, Mohebbi N, Khoshnevisan A. Role of dimethyl fumarate in the treatment of glioblastoma multiforme: A review article. Iran J Neurol. 2019;18(3):127-33. https://doi.org/10.18502/ijnl.v18i3.1636PMid:31749934 PMCid:PMC6858600 Saidu NEB, Kavian N, Leroy K, Jacob C, Nicco C, Batteux F, et al. Dimethyl fumarate, a two-edged drug: Current status and future directions. Med Res Rev. 2019;39(5):1923-52. https://doi.org/10.1002/med.21567PMid:30756407 Loewe R, Valero T, Kremling S, Pratscher B, Kunstfeld R, Pehamberger H, et al. Dimethylfumarate impairs melanoma growth and metastasis. Cancer Res. 2006;66(24):11888-96. https://doi.org/10.1158/0008-5472.CAN-06-2397PMid:17178886 Kastrati I, Siklos MI, Calderon-Gierszal EL, El-Shennawy L, Georgieva G, Thayer EN, et al. Dimethyl Fumarate Inhibits the Nuclear Factor κB Pathway in Breast Cancer Cells by Covalent Modification of p65 Protein. J Biol Chem. 2016;291(7):3639-47. https://doi.org/10.1074/jbc.M115.679704PMid:26683377 PMCid:PMC4751401 Han G, Zhou Q. Dimethylfumarate induces cell cycle arrest and apoptosis via regulating intracellular redox systems in HeLa cells. In Vitro Cell Dev Biol Anim. 2016;52(10):1034-41. https://doi.org/10.1007/s11626-016-0069-2PMid:27496192 Xie X, Zhao Y, Ma CY, Xu XM, Zhang YQ, Wang CG, et al. Dimethyl fumarate induces necroptosis in colon cancer cells through GSH depletion/ROS increase/MAPKs activation pathway. Br J Pharmacol. 2015;172(15):3929-43. https://doi.org/10.1111/bph.13184PMid:25953698 PMCid:PMC4523346 Gu B, DeAngelis LM. Enhanced cytotoxicity of bioreductive antitumor agents with dimethyl fumarate in human glioblastoma cells. Anticancer Drugs. 2005;16(2):167-74. https://doi.org/10.1097/00001813-200502000-00008PMid:15655414 Bennett Saidu NE, Bretagne M, Mansuet AL, Just PA, Leroy K, Cerles O, et al. Dimethyl fumarate is highly cytotoxic in KRAS mutated cancer cells but spares non-tumorigenic cells. Oncotarget. 2018;9(10):9088-99. https://doi.org/10.18632/oncotarget.24144PMid:29507676 PMCid:PMC5823659 Jadhav V, Solaroglu I, Obenaus A, Zhang JH. Neuroprotection against surgically induced brain injury. Surg Neurol. 2007;67(1):15-20. https://doi.org/10.1016/j.surneu.2006.07.014PMid:17210286 PMCid:PMC1852449 Kapural M, Krizanac-Bengez L, Barnett G, Perl J, Masaryk T, Apollo D, et al. Serum S-100beta as a possible marker of blood-brain barrier disruption. Brain Res. 2002;940(1-2):102-4. https://doi.org/10.1016/S0006-8993(02)02586-6 Guerra WK, Gaab MR, Dietz H, Mueller JU, Piek J, Fritsch MJ. Surgical decompression for traumatic brain swelling: indications and results. J Neurosurg. 1999;90(2):187-96. https://doi.org/10.3171/jns.1999.90.2.0187PMid:9950487 Shafer D, Tombes MB, Shrader E, Ryan A, Bandyopadhyay D, Dent P, et al. Phase I trial of dimethyl fumarate, temozolomide, and radiation therapy in glioblastoma. Neurooncol Adv. 2020;2(1):vdz052-vdz. https://doi.org/10.1093/noajnl/vdz052PMid:32642720 PMCid:PMC7212848 Shabani M, Taghvaei Javanshir H, Bereimipour A, Ebrahimi Sadrabadi A, Jalili A, Nayernia K. Contradictory Effect of Notch1 and Notch2 on Phosphatase and Tensin Homolog and its Influence on Glioblastoma Angiogenesis. Galen Med J. 2021;10(0):e2091. https://doi.org/10.31661/gmj.v10i0.2091 Bruder N, Ravussin P. Recovery from anesthesia and post-operative extubation of neurosurgical patients: a review. J Neurosurg Anesthesiol. 1999;11(4):282-93. https://doi.org/10.1097/00008506-199910000-00009PMid:10527148 Gerzeny M, Cohen AR. Advances in endoscopic neurosurgery. AORN J. 1998;67(5):957-61, 63-5. https://doi.org/10.1016/S0001-2092(06)62621-5 Patel CK, Vemaraju R, Glasbey J, Shires J, Northmore T, Zaben M, et al. Trends in peri-operative performance status following resection of high grade glioma and brain metastases: The impact on survival. Clin Neurol Neurosurg. 2018;164:67-71. https://doi.org/10.1016/j.clineuro.2017.11.016PMid:29197281 Sacko A, Hou MM, Temgoua M, Alkhafaji A, Marantidou A, Belin C, et al. Evolution of the Karnosky Performance Status throughout life in glioblastoma patients. Neuro Oncol. 2015;122(3):567-73. https://doi.org/10.1007/s11060-015-1749-6PMid:25700836 Chambless LB, Kistka HM, Parker SL, Hassam-Malani L, McGirt MJ, Thompson RC. The relative value of post-operative versus preoperative Karnofsky Performance Scale scores as a predictor of survival after surgical resection of glioblastoma multiforme. Neuro Oncol. 2015;121(2):359-64. https://doi.org/10.1007/s11060-014-1640-xPMid:25344883 Kowalczuk A, Macdonald RL, Amidei C, Dohrmann G, 3rd, Erickson RK, Hekmatpanah J, et al. Quantitative imaging study of extent of surgical resection and prognosis of malignant astrocytomas. Neurosurgery. 1997;41(5):1028-36; discussion 36-8. https://doi.org/10.1097/00006123-199711000-00004PMid:9361056