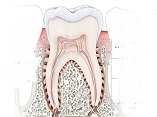
In Vitro Effects of Photobiomodulation with 660 Nm Laser and Vitamin D on Osteoblastic Differentiation of Human Periodontal Ligament Stem Cells
Photobiomodulation Laser and Vitamin D on Osteoblastic Differentiation of Periodontal Ligament Stem Cells
DOI:
https://doi.org/10.31661/gmj.v13i.3312Keywords:
Photobiomodulation Therapy; Mesenchymal Stem Cells; Cell Differentiations; Cellular Engineering; Vitamin DAbstract
Background: Mesenchymal stem cells (MSCs) can be found inside the human periodontal ligament. Application of vitamin D and photobiomodulation for regulation of the proliferation of MSCs and bone differentiation have been recently considered in cell engineering. This study is performed to evaluate the effects of photobiomodulation with 660 nm laser exposure and vitamin D on human periodontal ligament stem cells (HPDLSCs) and their osteoblastic differentiation properties. Materials and Methods: This study, was an in vitro experimental study performed on HPDLSCs in six groups of (I) control cells in the culture medium with no intervention, (II) addition of 10-7 mol vitamin D to the medium, (III) 660 nm diode laser exposure in 3 J/cm2 density of energy, (IV) 660 nm diode laser exposure in 3 J/cm2 density of energy + addition of 10-7 mol vitamin D to the medium, (V) 660 nm diode laser exposure in 5 J/cm2 density of energy, and (VI) 660 nm diode laser exposure in 5 J/cm2 density of energy + addition of 10-7 mol vitamin D to the medium. after 24 hours of the last exposure, cell viability had been assessed by methyl thiazolyl tetrazolium assay. The expression of Runt-related transcription factor 2 (RUNX2), osteopontin (OPN), alkaline phosphatase (ALP), and osteocalcin (OCN) genes was also assessed by reverse transcription-polymerase chain reaction, then Alizarin red staining was used to assess calcification. Results: Combined use of 660 nm laser with 3 and 5 J/cm2 density of energy and 10-7 mol vitamin D significantly increased cell viability, osteoblastic differentiation by upregulation of RUNX2, ALP, OPN, and OCN, and calcification (P<0.05). Conclusion: The results showed that combined use of vitamin D3 and irradiation of 660 nm laser with 3 J/cm2 and particularly 5 J/cm2 energy density increased the viability of HPDLSCs and enhanced their osteoblastic differentiation.
References
Zhang ZY, Teoh SH, Hui JH, Fisk NM, Choolani M, Chan JK. The potential of human fetal mesenchymal stem cells for off-the-shelf bone tissue engineering application. Biomaterials. 2012 Mar;33(9):2656-72.
https://doi.org/10.1016/j.biomaterials.2011.12.025
PMid:22217806
Naderi H, Matin MM, Bahrami AR. Review paper: critical issues in tissue engineering: biomaterials, cell sources, angiogenesis, and drug delivery systems. J Biomater Appl. 2011 Nov;26(4):383-417.
https://doi.org/10.1177/0885328211408946
PMid:21926148
Abdelgawad LM, Abdelaziz AM, Sabry D, Abdelgwad M. Influence of photobiomodulation and vitamin D on osteoblastic differentiation of human periodontal ligament stem cells and bone-like tissue formation through enzymatic activity and gene expression. Biomol Concepts. 2020 Dec 23;11(1):172-181.
https://doi.org/10.1515/bmc-2020-0016
PMid:34233429
Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, Young M, Robey PG, Wang CY, Shi S. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004 Jul 10-16;364(9429):149-55.
https://doi.org/10.1016/S0140-6736(04)16627-0
PMid:15246727
Chen FM, Jin Y. Periodontal tissue engineering and regeneration: current approaches and expanding opportunities. Tissue Eng Part B Rev. 2010 Apr;16(2):219-55.
https://doi.org/10.1089/ten.teb.2009.0562
PMid:19860551
Pinheiro CCG, de Pinho MC, Aranha AC, Fregnani E, Bueno DF. Low Power Laser Therapy: A Strategy to Promote the Osteogenic Differentiation of Deciduous Dental Pulp Stem Cells from Cleft Lip and Palate Patients. Tissue Eng Part A. 2018 Apr;24(7-8):569-575.
https://doi.org/10.1089/ten.tea.2017.0115
PMid:28699387
Lichtenstein A, Ferreira-Júnior M, Sales MM, Aguiar FB, Fonseca LA, Sumita NM, Duarte AJ; Grupo de Estudos para o Uso Racional do Laboratório Clínico do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo. Vitamin D: non-skeletal actions and rational use. Rev Assoc Med Bras (1992). 2013 Sep-Oct;59(5):495-506.
Posa F, Di Benedetto A, Colaianni G, Cavalcanti-Adam EA, Brunetti G, Porro C, Trotta T, Grano M, Mori G. Vitamin D Effects on Osteoblastic Differentiation of Mesenchymal Stem Cells from Dental Tissues. Stem Cells Int. 2016;2016:9150819.
https://doi.org/10.1155/2016/9150819
PMid:27956902 PMCid:PMC5124467
Sajedi SM, Abbasi F, Asnaashari M, Jafarian AA. Comparative Efficacy of Low-Level Laser Acupuncture and Cupping for Treatment of Patients with Myofascial Pain Dysfunction Syndrome: A Double-blinded, Randomized Clinical Trial: Comparison of the Effects of LLL Acupuncture and Cupping. Galen Medical Journal. 2022;11:1.Ferlito JV, Silva CF, Almeida JC, da Silva Lopes IA, da Silva Almeida R, Leal-Junior ECP, De Marchi T. Effects of photobiomodulation therapy (PBMT) on the management of pain intensity and disability in plantar fasciitis: systematic review and meta-analysis. Lasers Med Sci. 2023 Jul 18;38(1):163.
https://doi.org/10.1007/s10103-023-03823-0
PMid:37464155
Posa F, Di Benedetto A, Cavalcanti-Adam EA, Colaianni G, Porro C, Trotta T, Brunetti G, Lo Muzio L, Grano M, Mori G. Vitamin D Promotes MSC Osteogenic Differentiation Stimulating Cell Adhesion and αVβ3 Expression. Stem Cells Int. 2018 Feb 28;2018:6958713.
https://doi.org/10.1155/2018/6958713
PMid:29681950 PMCid:PMC5851411
Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015 Apr;33(4):183-4.
https://doi.org/10.1089/pho.2015.9848
PMid:25844681 PMCid:PMC4390214
Hosseinpour S, Fekrazad R, Arany PR, Ye Q. Molecular impacts of photobiomodulation on bone regeneration: A systematic review. Prog Biophys Mol Biol. 2019 Dec;149:147-159.
https://doi.org/10.1016/j.pbiomolbio.2019.04.005
PMid:31002851
Song I, Kim BS, Kim CS, Im GI. Effects of BMP-2 and vitamin D3 on the osteogenic differentiation of adipose stem cells. Biochem Biophys Res Commun. 2011 Apr 29;408(1):126-31.
https://doi.org/10.1016/j.bbrc.2011.03.135
PMid:21463608
Liu M, Xu H, Ma Y, Cheng J, Hua Z, Huang G. Osteoblasts Proliferation and Differentiation Stimulating Activities of the Main Components of Epimedii folium. Pharmacogn Mag. 2017 Jan-Mar;13(49):90-94.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, Moorman MA, Simonetti DW, Craig S, Marshak DR. Multilineage potential of adult human mesenchymal stem cells. Science. 1999 Apr 2;284(5411):143-7.
https://doi.org/10.1126/science.284.5411.143
PMid:10102814
Pinheiro CC, Bueno DF. Alternative strategies for stem cell osteogenic differentiation. InOsteogenesis and Bone Regeneration: IntechOpen; 2018 .
Kreisler M, Christoffers AB, Willershausen B, d'Hoedt B. Effect of low-level GaAlAs laser irradiation on the proliferation rate of human periodontal ligament fibroblasts: an in vitro study. J Clin Periodontol. 2003 Apr;30(4):353-8.
https://doi.org/10.1034/j.1600-051X.2003.00001.x
PMid:12694435
Choi EJ, Yim JY, Koo KT, Seol YJ, Lee YM, Ku Y, Rhyu IC, Chung CP, Kim TI. Biological effects of a semiconductor diode laser on human periodontal ligament fibroblasts. J Periodontal Implant Sci. 2010 Jun;40(3):105-10.
https://doi.org/10.5051/jpis.2010.40.3.105
PMid:20607054 PMCid:PMC2895515
Wu JY, Chen CH, Yeh LY, Yeh ML, Ting CC, Wang YH. Low-power laser irradiation promotes the proliferation and osteogenic differentiation of human periodontal ligament cells via cyclic adenosine monophosphate. Int J Oral Sci. 2013 Jun;5(2):85-91.
https://doi.org/10.1038/ijos.2013.38
PMid:23788285 PMCid:PMC3707076
Bouvet-Gerbettaz S, Merigo E, Rocca JP, Carle GF, Rochet N. Effects of low-level laser therapy on proliferation and differentiation of murine bone marrow cells into osteoblasts and osteoclasts. Lasers Surg Med. 2009 Apr;41(4):291-7.
https://doi.org/10.1002/lsm.20759
PMid:19347941
Peng F, Wu H, Zheng Y, Xu X, Yu J. The effect of noncoherent red light irradiation on proliferation and osteogenic differentiation of bone marrow mesenchymal stem cells. Lasers Med Sci. 2012 May;27(3):645-53.
https://doi.org/10.1007/s10103-011-1005-z
PMid:22016038
Ji Y, Zhang P, Xing Y, Jia L, Zhang Y, Jia T, Wu X, Zhao B, Xu X. Effect of 1α, 25-dihydroxyvitamin D3 on the osteogenic differentiation of human periodontal ligament stem cells and the underlying regulatory mechanism. Int J Mol Med. 2019 Jan;43(1):167-176.
https://doi.org/10.3892/ijmm.2018.3947
Wang YL, Hong A, Yen TH, Hong HH. Isolation of Mesenchymal Stem Cells from Human Alveolar Periosteum and Effects of Vitamin D on Osteogenic Activity of Periosteum-derived Cells. J Vis Exp. 2018 May 4;(135):57166.
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







