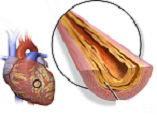
Characterization of Atherosclerotic Plaque in Coronary CT Angiography and Some Related Factors in Patients with Coronary Artery Disease Referred to Farshchian Heart Hospital in Hamadan in 2023
DOI:
https://doi.org/10.31661/gmj.vi.3702Keywords:
Coronary Vessels; Atherosclerotic Plaque; Coronary AngiographyAbstract
Background: Vascular classification in coronary artery disease is influenced by atherosclerotic plaque characteristics. This study aimed to investigate the characterization of atherosclerotic plaque and some related factors in coronary CT angiography in patients with coronary artery disease referred to Farshchian Heart Hospital in Hamadan in 2023. Materials and Methods: In this analytical cross-sectional study that was conducted in 2023 in Hamadan, Iran, 140 individuals suspected of coronary artery stenosis based on atherosclerotic plaque characteristics in coronary angiography were examined. The study analyzed the relationship between plaque features, demographic characteristics, degree of coronary artery stenosis, and other risk factors for coronary artery disease with chi-square, logistic regression, correlation coefficient using SPSS version 20. Results: The mean age of patients was 53.11±7.62 years, with 59% male and 40% female. Among patients, 40% had coronary artery stenosis, with 18% having severe stenosis. The prevalence of positive remodeling was 32%, Low Attenuation was 45%, Napkin-ring Sign was 14%, and Spotty Calcium was 25%. Significant associations were found between various plaque patterns and age (P<0.05), Low Attenuation pattern with hypertension (P<0.001), diabetes (P=0.03), dyslipidemia (P=0.04), Napkin-ring Sign with diabetes (P=0.03). Conclusion: The study highlights the high prevalence of distinct plaque patterns and their associations with severity of coronary artery stenosis, presence of diabetes, hypertension, and dyslipidemia. These findings emphasize the need for tailored risk assessment and management strategies in patients with coronary artery disease.
References
Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS et al. Atherosclerosis. Nature Reviews Disease Primers. 2019;5(1):56.
https://doi.org/10.1038/s41572-019-0106-z
PMid:31420554
Jamee Shahwan A, Abed Y, Desormais I, Magne J, Preux PM, Aboyans V et al. Epidemiology of coronary artery disease and stroke and associated risk factors in Gaza community -Palestine. PLOS ONE. 2019;14(1):e0211131.
https://doi.org/10.1371/journal.pone.0211131
PMid:30682090 PMCid:PMC6347168
Mendis S, Puska P, Norrving Be, Organization WH. Global atlas on cardiovascular. disease prevention and control: World Health Organization; 2011.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146-e603.
https://doi.org/10.1161/CIR.0000000000000491
Hajar R. Risk Factors for Coronary Artery Disease: Historical Perspectives. Heart Views. 2017;18(3):109-14.
https://doi.org/10.4103/HEARTVIEWS.HEARTVIEWS_106_17
PMid:29184622 PMCid:PMC5686931
Maurovich-Horvat P, Ferencik M, Voros S, Merkely B, Hoffmann U. Comprehensive plaque assessment by coronary CT angiography. Nature Reviews Cardiology. 2014;11(7):390-402.
https://doi.org/10.1038/nrcardio.2014.60
PMid:24755916
Achenbach S, Raggi P. Imaging of coronary atherosclerosis by computed tomography. European Heart Journal. 2010;31(12):1442-8.
https://doi.org/10.1093/eurheartj/ehq150
PMid:20484566
Klass O, Kleinhans S, Walker MJ, Olszewski M, Feuerlein S, Juchems M et al. Coronary plaque imaging with 256-slice multidetector computed tomography: interobserver variability of volumetric lesion parameters with semiautomatic plaque analysis software. The International Journal of Cardiovascular Imaging. 2010;26(6):711-20.
https://doi.org/10.1007/s10554-010-9614-3
PMid:20339922
Voros S, Rinehart S, Qian Z, Joshi P, Vazquez G, Fischer C et al. Coronary atherosclerosis imaging by coronary CT angiography: current status, correlation with intravascular interrogation and meta-analysis. JACC Cardiovasc Imaging. 2011;4(5):537-48.
https://doi.org/10.1016/j.jcmg.2011.03.006
PMid:21565743
Nakazato R, Otake H, Konishi A, Iwasaki M, Koo B-K, Fukuya H et al. Atherosclerotic plaque characterization by CT angiography for identification of high-risk coronary artery lesions: a comparison to optical coherence tomography. European Heart Journal - Cardiovascular Imaging. 2014;16(4):373-9.
https://doi.org/10.1093/ehjci/jeu188
PMid:25246503
Bittner DO, Mayrhofer T, Puchner SB, Lu MT, Maurovich-Horvat P, Ghemigian K et al. Coronary Computed Tomography Angiography-Specific Definitions of High-Risk Plaque Features Improve Detection of Acute Coronary Syndrome. Circulation: Cardiovascular Imaging. 2018;11(8):e007657.
https://doi.org/10.1161/CIRCIMAGING.118.007657
PMid:30354493 PMCid:PMC6205220
Kataoka Y, Wolski K, Uno K, Puri R, Tuzcu EM, Nissen SE et al. Spotty Calcification as a Marker of Accelerated Progression of Coronary Atherosclerosis. Journal of the American College of Cardiology. 2012;59(18):1592-7.
https://doi.org/10.1016/j.jacc.2012.03.012
PMid:22538329
Finck T, Stojanovic A, Will A, Hendrich E, Martinoff S, Hausleiter J, et al. Long-term prognostic value of morphological plaque features on coronary computed tomography angiography. European Heart Journal-Cardiovascular Imaging. 2020;21(3):237-48.
https://doi.org/10.1093/ehjci/jez238
PMid:31578556
Jadidi M, Poulson W, Aylward P, MacTaggart J, Sanderfer C, Marmie B et al. Calcification prevalence in different vascular zones and its association with demographics, risk factors, and morphometry. American Journal of Physiology-Heart and Circulatory Physiology. 2021;320(6):H2313-H23.
https://doi.org/10.1152/ajpheart.00040.2021
PMid:33961507 PMCid:PMC8289361
Khalagi K, Mansournia MA, Motevalian S-A, Nourijelyani K, Rahimi-Movaghar A, Bakhtiyari M. An ad hoc method for dual adjusting for measurement errors and nonresponse bias for estimating prevalence in survey data: Application to Iranian mental health survey on any illicit drug use. Statistical Methods in Medical Research. 2018;27(10):3062-76.
https://doi.org/10.1177/0962280217690939
PMid:29298600
Stovitz SD, Banack HR, Kaufman JS. Selection bias can creep into unselected cohorts and produce counterintuitive findings. International Journal of Obesity. 2021;45(1):276-7.
https://doi.org/10.1038/s41366-020-00720-2
PMid:33235356
Pakzad R, Nedjat S, Salehiniya H, Mansournia N, Etminan M, Nazemipour M et al. Effect of alcohol consumption on breast cancer: probabilistic bias analysis for adjustment of exposure misclassification bias and confounders. BMC Medical Research Methodology. 2023;23(1):157.
https://doi.org/10.1186/s12874-023-01978-6
PMid:37403100 PMCid:PMC10318777
Moradzadeh R, Mansournia MA, Ghiasvand R, Baghfalaki T, Nadrian H, Holakouie-Naieni K. Impact of Age at Menarche on Breast Cancer: The Assessment of Recall Bias. Arch Iran Med. 2019;22(2):65-70.
Moradzadeh R, Mansournia MA, Baghfalaki T, Nadrian H, Gustafson P, McCandless LC. The impact of maternal smoking during pregnancy on childhood asthma: adjusted for exposure misclassification; results from the National Health and Nutrition Examination Survey, 2011-2012. Annals of Epidemiology. 2018;28(10):697-703.
https://doi.org/10.1016/j.annepidem.2018.07.011
PMid:30150159
Nazari J, Chezani-Sharahi N, Eshrati B, Yadegari A, Naghshbandi M, Movahedi H et al. Prevalence and determinants of self-medication consumption of antibiotics in children in Iran: A population-based cross-sectional study, 2018-19. PLOS ONE. 2022;17(12):e0278843.
https://doi.org/10.1371/journal.pone.0278843
PMid:36584040 PMCid:PMC9803171
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







