Dual Primary Gastric and Rectal Adenocarcinoma: A Case Report with Management Insights
DOI:
https://doi.org/10.31661/gmj.v14i.3742Keywords:
Dual Primary Malignancies; Colorectal Cancer; Gastric Cancer; Metachronous; Synchronous; Multidisciplinary TeamAbstract
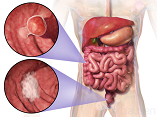
Background: Dual primary malignancies, including colorectal (CRC) and gastric cancers (GC), are complicated cases due to the complexity of managing patients. Case Report: This case report presents a 62-year-old male patient with rectal and gastric adenocarcinomas. Initially, rectal adenocarcinoma after a complaint of hematochezia was diagnosed by prognostic modalities. The patient received total neoadjuvant therapy with FOLFOX chemotherapy and chemoradiotherapy. After surgery, a complete pathological response was obtained. A few months later, gastric adenocarcinoma with persistent heartburn was detected through esophagogastroduodenoscopy (EGD). total neoadjuvant therapy with FOLFOX chemotherapy and chemoradiotherapy followed by total gastrectomy were prescribed. After gastrectomy, a complete pathological response was obtained. Conclusion: This case of synchronous CRC and GC, diagnosed 5 months apart, underscores the pivotal role of early detection and multidisciplinary management in achieving favorable outcomes. Complete pathologic responses in both malignancies following tailored TNT with FOLFOX and FLOT regimens, combined with surgical interventions, highlight the efficacy of personalized treatment strategies, even in resource-constrained settings. Continued research is essential to optimize diagnostic protocols, refine therapeutic approaches, and improve access to genetic testing for synchronous and metachronous malignancies, promoting equitable cancer care globally.
References
Warren S, Gates O. Multiple primary malignant tumors A survey of the literature and a statistical study. Am J cancer. 1932;16:1358-414.
Suzuki T, Takahashi H, Yao K, Inagi K, Nakayama M, Makoshi T et al. Multiple primary malignancies in the head and neck: a clinical review of 121 patients. Acta Oto-Laryngologica. 2002;122(4):88-92.
https://doi.org/10.1080/000164802760057662
PMid:12212604
Artac M, Bozcuk H, Ozdogan M, Demiral AN, Sarper A, Samur M et al. Different clinical features of primary and secondary tumors in patients with multiple malignancies. Tumori Journal. 2005;91(4):317-20.
https://doi.org/10.1177/030089160509100406
PMid:16277096
Demandante CG, Troyer DA, Miles TP. Multiple primary malignant neoplasms: case report and a comprehensive review of the literature. American journal of clinical oncology. 2003;26(1):79-83.
https://doi.org/10.1097/00000421-200302000-00015
PMid:12576929
Tachimori Y. Cancer screening in patients with cancer. Japanese journal of clinical oncology. 2002 Apr 1;32(4):118-9.
https://doi.org/10.1093/jjco/hyf042
PMid:12072420
Ferlay J EM, Lam F, Laversanne M, Colombet M, Mery L, Piñeros M, Znaor A, Soerjomataram I, Bray F. Lyon, France: International Agency for Research on Cancer, Global Cancer Observatory: Cancer Today (version 1.1). 2024.
Lee JH, Bae JS, Ryu KW, Lee JS, Park SR, Kim CG et al. Gastric cancer patients at high-risk of having synchronous cancer. World journal of gastroenterology. 2006;12(16):2588-92.
https://doi.org/10.3748/wjg.v12.i16.2588
PMid:16688807 PMCid:PMC4087994
Lim SB, Jeong SY, Choi HS, Sohn DK, Hong CW, Jung KH et al. Synchronous gastric cancer in primary sporadic colorectal cancer patients in Korea. International journal of colorectal disease. 2008;23(1):61-5.
https://doi.org/10.1007/s00384-007-0366-z
PMid:17724601
Yoon SN, Oh ST, Lim SB, Kim TW, Kim JH, Yu CS et al. Clinicopathologic characteristics of colorectal cancer patients with synchronous and metachronous gastric cancer. World journal of surgery. 2010;34(9):2168-76.
https://doi.org/10.1007/s00268-010-0623-0
PMid:20532772
Saito S, Hosoya Y, Togashi K, Kurashina K, Haruta H, Hyodo M et al. Prevalence of synchronous colorectal neoplasms detected by colonoscopy in patients with gastric cancer. Surgery today. 2008;38:20-5.
https://doi.org/10.1007/s00595-007-3567-8
PMid:18085357
Lin Y-J, Chen H-X, Zhang F-X, Hu X-S, Huang H-J, Lu J-H et al. Features of synchronous and metachronous dual primary gastric and colorectal cancer. World Journal of Gastrointestinal Oncology. 2023;15(11):1864.
https://doi.org/10.4251/wjgo.v15.i11.1864
PMid:38077635 PMCid:PMC10701232
Park J-H, Baek J-H, Yang J-Y, Lee W-S, Lee W-K. Clinicopathologic characteristics and survival rate in patients with synchronous or metachronous double primary colorectal and gastric cancer. Korean Journal of Clinical Oncology. 2018;14(2):83-8.
https://doi.org/10.14216/kjco.18015
Engstrand J, Strömberg C, Nilsson H, Freedman J, Jonas E. Synchronous and metachronous liver metastases in patients with colorectal cancer-towards a clinically relevant definition. World Journal of Surgical Oncology. 2019;17(1):228.
https://doi.org/10.1186/s12957-019-1771-9
PMid:31878952 PMCid:PMC6933908
Tanjak P, Suktitipat B, Vorasan N, Juengwiwattanakitti P, Thiengtrong B, Songjang C et al. Risks and cancer associations of metachronous and synchronous multiple primary cancers: a 25-year retrospective study. BMC Cancer. 2021;21(1):1045.
https://doi.org/10.1186/s12885-021-08766-9
PMid:34556087 PMCid:PMC8461969
Flor N, Zanchetta E, Di Leo G, Mezzanzanica M, Greco M, Carrafiello G, et al. Synchronous colorectal cancer using CT colonography vs other means: a systematic review and meta-analysis. Abdominal radiology (New York). 2018;43(12):3241-9.
https://doi.org/10.1007/s00261-018-1658-1
PMid:29948053
He W, Zheng C, Wang Y, Dan J, Zhu M, Wei M et al. Prognosis of synchronous colorectal carcinoma compared to solitary colorectal carcinoma: a matched pair analysis. European journal of gastroenterology & hepatology. 2019;31(12):1489-95.
https://doi.org/10.1097/MEG.0000000000001487
PMid:31441800 PMCid:PMC6844654
Benson AB, Venook AP, Adam M, Chang G, Chen Y-J, Ciombor KK et al. NCCN Guidelines® Insights: Rectal Cancer, Version 3.2024: Featured Updates to the NCCN Guidelines. Journal of the National Comprehensive Cancer Network. 2024;22(6):366-75.
https://doi.org/10.6004/jnccn.2024.0041
PMid:39151454
Cervantes A, Adam R, Roselló S, Arnold D, Normanno N, Taïeb J et al. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Annals of Oncology. 2023;34(1):10-32.
https://doi.org/10.1016/j.annonc.2022.10.003
PMid:36307056
Atay-Rosenthal S, Wahl RL, Fishman EK. PET/CT findings in gastric cancer: potential advantages and current limitations. Imaging in Medicine. 2012;4(2):241.
https://doi.org/10.2217/iim.12.5
Shenoy S. Synchronous gastric and colon cancers: Important to consider hereditary syndromes and chronic inflammatory disease associations. World J Gastrointest Oncol. 2024;16(3):571-6.
https://doi.org/10.4251/wjgo.v16.i3.571
PMid:38577475 PMCid:PMC10989375
Ajose AO, Graef K, Mallum AA, Oladipo A, Ibrahim F, Li H et al. Genetic testing in cancer care: An assessment of current practice in Africa. Journal of Clinical Oncology. 2024;42(16_suppl):e13784-e.
https://doi.org/10.1200/JCO.2024.42.16_suppl.e13784
The Lancet O. Meeting the need for germline testing. The Lancet Oncology. 2023;24(7):709.
https://doi.org/10.1016/S1470-2045(23)00295-4
PMid:37414006
Ho V, Chung L, Lim SH, Ma Y, Wang B, Lea V et al. Prognostic Impact of TP53 Mutations and Tumor Mutational Load in Colorectal Cancer. Gastrointestinal Disorders. 2022;4(3):165-79.
https://doi.org/10.3390/gidisord4030016
Infante M, Arranz-Ledo M, Lastra E, Olaverri A, Ferreira R, Orozco M et al. Profiling of the genetic features of patients with breast, ovarian, colorectal and extracolonic cancers: Association to CHEK2 and PALB2 germline mutations. Clinica chimica acta; international journal of clinical chemistry. 2024;552:117695.
https://doi.org/10.1016/j.cca.2023.117695
PMid:38061684
Li Y, Liu H, Li T, Feng J, He Y, Chen L et al. Choroid Plexus Carcinomas With TP53 Germline Mutations: Management and Outcome. Frontiers in oncology. 2021;11:751784.
https://doi.org/10.3389/fonc.2021.751784
PMid:34660315 PMCid:PMC8514937
Farrokhi P, Sadeghi A, Sharifi M, Riechelmann R, Moghaddas A. Efficacy and safety of FLOT regimen vs DCF, FOLFOX, and ECF regimens as perioperative chemotherapy treatments for resectable gastric cancer patients; a report from the middle east. Research in pharmaceutical sciences. 2022;17(6):621-34.
https://doi.org/10.4103/1735-5362.359430
PMid:36704436 PMCid:PMC9872182
Möhring C, Timotheou A, Mańczak A, Sadeghlar F, Zhou T, Mahn R et al. Efficacy and tolerability of fluorouracil, leucovorin, oxaliplatin and docetaxel (FLOT) in unselected patients with advanced gastric and gastroesophageal cancer: does age really matter? Journal of cancer research and clinical oncology. 2023;149(5):1849-62.
https://doi.org/10.1007/s00432-022-04109-8
PMid:35763109
Tastekin D, Paksoy N, Dogan I, Ferhatoglu F, Khanmammadov N, Bozbey HU, et al. Fluorouracil, leucovorin, oxaliplatin, and docetaxel (FLOT) regimen in the first-line treatment of metastatic gastric cancer: A single-center experience. J Cancer Res Ther. 2023 Jan-Mar;19(2):253-258.
https://doi.org/10.4103/jcrt.jcrt_672_22
PMid:37006064
Dos Santos M, Lequesne J, Leconte A, Corbinais S, Parzy A, Guilloit J-M et al. Perioperative treatment in resectable gastric cancer with spartalizumab in combination with fluorouracil, leucovorin, oxaliplatin and docetaxel (FLOT): a phase II study (GASPAR). BMC Cancer. 2022;22(1):537.
https://doi.org/10.1186/s12885-022-09623-z
PMid:35549674 PMCid:PMC9097175
Sah BK, Zhang B, Zhang H, Li J, Yuan F, Ma T et al. Neoadjuvant FLOT versus SOX phase II randomized clinical trial for patients with locally advanced gastric cancer. Nature Communications. 2020;11(1):6093.
https://doi.org/10.1038/s41467-020-19965-6
PMid:33257672 PMCid:PMC7705676
Anghelone A, Bensi M, Barbaro B, Calegari MA, Cina C, Menghi R, et al. The impact of the multidisciplinary team (MDT) in the management of colorectal cancer (CRC).
Layfield DM, Flashman KG, Benitez Majano S, Senapati A, Ball C, Conti JA et al. Changing patterns of multidisciplinary team treatment, early mortality, and survival in colorectal cancer. BJS open. 2022;6(5).
https://doi.org/10.1093/bjsopen/zrac098
PMid:36254731 PMCid:PMC9577547
Mangone L, Zizzo M, Nardecchia M, Marinelli F, Bisceglia I, Braghiroli MB et al. Impact of Multidisciplinary Team Management on Survival and Recurrence in Stage I-III Colorectal Cancer: A Population-Based Study in Northern Italy. Biology. 2024;13(11):928.
https://doi.org/10.3390/biology13110928
PMid:39596883 PMCid:PMC11592292
Ostroff C. Multidisciplinary teams and social science: a patient perspective. Colorectal Disease. 2024;26(5):1061-7.
https://doi.org/10.1111/codi.16957
PMid:38519855
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







