Effect of Innovative Low-level Laser Therapy Protocol for Stress Urinary Incontinence: A Case Series Study
DOI:
https://doi.org/10.31661/gmj.v14i.3841Abstract
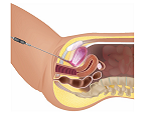
Stress urinary incontinence (SUI) is a prevalent condition characterized by involuntary urine leakage during physical activities. This condition can significantly impact a woman’s quality of life. Treatment options for SUI include behavioral therapy, medication, and surgery. However, non-pharmacological methods such as low-level laser therapy (LLT) have demonstrated the potential to promote tissue repair, reduce inflammation, and improve pelvic floor muscle function in various pelvic floor disorders. Despite these benefits, the effectiveness of combined transvaginal and intra-bladder LLT for managing SUI has not been extensively studied. This case series aimed to assess the safety and efficacy of a novel regimen using concurrent transvaginal and intra-bladder LLT for the treatment of stress urinary incontinence in perimenopausal and postmenopausal women. The results appear promising, and further investigation is recommended. Trial Registration: This clinical trial was registered in the Iranian Registry of Clinical Trials (IRCT) under the registration number IRCT20231203060255N2, on 30 June 2024 (retrospectively registered).
References
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein AJ. The standardization of terminology of lower urinary tract function: report from the standardization sub-committee of International Continence Society. InTextbook of female urology and urogynecology 2010 Jul 15 (pp. 1098-1108). CRC Press.
https://doi.org/10.3109/9781439807217-110
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318(16):1592-1604.
https://doi.org/10.1001/jama.2017.12137
PMid:29067433
Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217-222.
https://doi.org/10.1080/13697137.2018.1543263
PMid:30572737
Dumoulin C, Cacciari LP, Hay-Smith EJ. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10:CD005654.
https://doi.org/10.1002/14651858.CD005654.pub4
PMid:30288727 PMCid:PMC6516955
Hamblin MR. Mechanisms and applications of the anti-inflammatory effects of photobiomodulation. AIMS Biophys. 2017;4(3):337-361.
https://doi.org/10.3934/biophy.2017.3.337
PMid:28748217 PMCid:PMC5523874
Enwemeka CS, Parker JC, Dowdy DS. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004;22(4):323-329.
https://doi.org/10.1089/pho.2004.22.323
PMid:15345176
Gaspar A, Addamo G, Brandi H. Vaginal fractional CO2 laser: a minimally invasive option for vaginal rejuvenation. Am J Cosmet Surg. 2011;28(3):156-162.
https://doi.org/10.1177/074880681102800309
Mousa G, Yousef A, El-Sayed R, El-Mekawy H, Sallam E, Hussein A, Hamada H. Effect of low-level laser on pelvic floor muscles and fascia in cases of stress urinary incontinence: a randomized controlled trial. Physiotherapy Quarterly. 2021 Oct 1;29(4):22-7.
https://doi.org/10.5114/pq.2021.102549
De Marchi T, Ferlito JV, Turra AC, Flamia S, de Bispo Magro F, Pavelecini Donida ML, Dilkin M, da Silva D, Massia Ribas V, Leal Junior EC. Pilates method and/or photobiomodulation therapy combined to static magnetic field in women with stress urinary incontinence: a randomized, double-blind, placebo-controlled clinical trial. Journal of Clinical Medicine. 2023 Jan 31;12(3):1104.
https://doi.org/10.3390/jcm12031104
PMid:36769752 PMCid:PMC9917687
Frederice CP, de Mira TA, Machado HC, Brito LG, Juliato CR. Effect of vaginal stretching and Photobiomodulation therapy on sexual function in women with pelvic floor Myofascial pain-A randomized clinical trial. The journal of sexual medicine. 2022 Jan;19(1):98-105.
https://doi.org/10.1016/j.jsxm.2021.10.008
PMid:34955173
Mousa G, Yousef A, El-Sayed R, El-Mekawy H, Sallam E, Hussein A, Hamada H. Effect of low level laser on pelvic floor muscles and fascia in cases of stress urinary incontinence: a randomized controlled trial. Physiotherapy Quarterly. 2021 Oct 1;29(4):22-7.
https://doi.org/10.5114/pq.2021.102549
Gaspar A, Addamo G, Brandi H. Vaginal fractional CO2 laser: a minimally invasive option for vaginal rejuvenation. The American Journal of Cosmetic Surgery. 2011 Sep;28(3):156-62.
https://doi.org/10.5992/0748-8068-28.3.156
Gambacciani M, Levancini M. Vaginal Erbium Laser: the second generation thermotherapy for the genitourinary syndrome of menopause (GSM) A pilot study. Maturitas. 2015 May 1;81(1):133.
https://doi.org/10.1016/j.maturitas.2015.02.105
Blaganje M, Šćepanović D, Žgur L, Verdenik I, Pajk F, Lukanović A. Non-ablative Er: YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2018 May 1;224:153-8.
https://doi.org/10.1016/j.ejogrb.2018.03.038
PMid:29604548
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







