The Interaction Between Orthodontics and Periodontal Tissue Remodeling
DOI:
https://doi.org/10.31661/gmj.vi.4005Keywords:
Orthodontics; Periodontal Remodeling; Tissue Engineering; Inflammation; Alveolar BoneAbstract
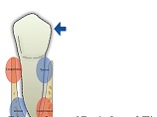
Orthodontic tooth movement (OTM) involves a complex cascade of biomechanical and biological events, orchestrated through the interaction of mechanical forces, inflammatory responses, and cellular remodeling within the periodontal ligament and alveolar bone. In adult patients, particularly those with a history of periodontitis, these processes are further complicated by reduced regenerative capacity, chronic inflammation, and altered bone dynamics. This review explores the mechanobiological foundations of OTM, detailing the roles of osteoclasts, osteoblasts, fibroblasts, and endothelial cells, as well as the central regulatory pathways, including RANKL/OPG signaling, cytokine cascades, and matrix metalloproteinase activity. Special attention is given to the clinical implications of orthodontic forces in healthy versus compromised periodontium, emphasizing the importance of force magnitude, direction, and regimen. Interdisciplinary coordination between orthodontists and periodontists is essential for safe and effective treatment planning, particularly when regenerative procedures such as bone grafting, guided tissue regeneration, or the use of biologics like enamel matrix derivative and platelet-rich fibrin are involved. The review also identifies critical knowledge gaps, including uncertainty regarding optimal treatment timing post-periodontal therapy, a lack of long-term and patient-centered outcomes, and the underrepresentation of adult-specific data in clinical research. Emerging technologies in tissue engineering, biomarker analysis, and digital orthodontic planning offer promising avenues for precision-based care. Ultimately, a collaborative, individualized approach that integrates biological insight with clinical expertise is key to achieving both periodontal stability and orthodontic success in periodontally vulnerable patients
References
Wang J, Huang Y, Chen F, Li W. The agerelated effects on orthodontic tooth movement and the surrounding periodontal environment. Front Physiol. 2024 Sept 6;15:1460168.
https://doi.org/10.3389/fphys.2024.1460168
PMid:39308977 PMCid:PMC11412856
Li B, Wang L, He H. Autophagy in orthodontic tooth movement: advances, challenges, and future perspectives. Mol Med. 2025 June 21;31(1):245.
https://doi.org/10.1186/s10020-025-01299-y
PMid:40544242 PMCid:PMC12181928
Li Y, Zhan Q, Bao M, Yi J, Li Y. Biomechanical and biological responses of periodontium in orthodontic tooth movement: update in a new decade. Int J Oral Sci. 2021 Dec;13(1):20.
https://doi.org/10.1038/s41368-021-00125-5
PMid:34183652 PMCid:PMC8239047
Zhong W, Zhou C, Yin Y, Feng G, Zhao Z, Pan Y, et al. Expert consensus on orthodontic treatment of patients with periodontal disease. Int J Oral Sci. 2025 Apr 3;17(1):27.
https://doi.org/10.1038/s41368-025-00356-w
PMid:40175337 PMCid:PMC11965299
Viglianisi G, Polizzi A, Lombardi T, Amato M, Grippaudo C, Isola G. Biomechanical and Biological Multidisciplinary Strategies in the Orthodontic Treatment of Patients with Periodontal Diseases: A Review of the Literature. Bioengineering. 2025 Jan 9;12(1):49.
https://doi.org/10.3390/bioengineering12010049
PMid:39851323 PMCid:PMC11760482
Oruba Z, Gibas-Stanek M, Pihut M, Cześnikiewicz-Guzik M, Stós W. Orthodontic treatment in patients with periodontitis - a narrative literature review. Aust Dent J. 2023 Dec;68(4):238-46.
https://doi.org/10.1111/adj.12974
PMid:37688346
Antonarakis GS, Zekeridou A, Kiliaridis S, Giannopoulou C. Periodontal considerations during orthodontic intrusion and extrusion in healthy and reduced periodontium. Periodontol 2000. 2024 June 3;prd:12578.
https://doi.org/10.1111/prd.12578
PMid:38831560
Saad NA, Ariffin F. Orthodontic and periodontal health interplay: insight from a case series. IIUM J Orofac Health Sci. 2025 Feb 28;6(1):147-59.
https://doi.org/10.31436/ijohs.v6i1.320
Feştilă D, Ciobotaru CD, Condurache P, Kahane L, Şimon CI, Chiş A, et al. Maintenance of periodontal health during adult orthodontic treatment. Med Evol. 2024 Sept 30;30(3):58694.
https://doi.org/10.70921/medev.v30i3.966
Alghamdi B, Jeon HH, Ni J, Qiu D, Liu A, Hong JJ, et al. Osteoimmunology in Periodontitis and Orthodontic Tooth Movement. Curr Osteoporos Rep. 2023 Apr;21(2):128-46.
https://doi.org/10.1007/s11914-023-00774-x
PMid:36862360 PMCid:PMC10696608
Maltha JC, KuijpersJagtman AM. Mechanobiology of orthodontic tooth movement: An update. J World Fed Orthod. 2023 Aug;12(4):156-60.
https://doi.org/10.1016/j.ejwf.2023.05.001
PMid:37349154
Zheng W, Lu X, Chen G, Shen Y, Huang X, Peng J, et al. The osteoclastic activity in apical distal region of molar mesial roots affects orthodontic tooth movement and root resorption in rats. Int J Oral Sci. 2024 Feb 28;16(1):19.
https://doi.org/10.1038/s41368-024-00284-1
PMid:38418457 PMCid:PMC10901898
Nakai Y, Praneetpong N, Ono W, Ono N. Mechanisms of Osteoclastogenesis in Orthodontic Tooth Movement and Orthodontically Induced Tooth Root Resorption. J Bone Metab. 2023 Nov 30;30(4):297-310.
https://doi.org/10.11005/jbm.2023.30.4.297
PMid:38073263 PMCid:PMC10721376
Yang CY, Jeon HH, Alshabab A, Lee YJ, Chung CH, Graves DT. RANKL deletion in periodontal ligament and bone lining cells blocks orthodontic tooth movement. Int J Oral Sci. 2018 Feb 26;10(1):3.
https://doi.org/10.1038/s41368-017-0004-8
PMid:29483595 PMCid:PMC5944595
Jamali S, Khosravi S, Shadmanpour M, Gharibpour F, Payahoo S, Darvish M. Hyalinization and Molecular Pathways Involved in Orthodontic Tooth Movement: A Systematic Review and MetaAnalysis. Pesqui Bras Em Odontopediatria E Clínica Integrada. 2020;20:e5408.
https://doi.org/10.1590/pboci.2020.148
Chaushu S, Klein Y, Mandelboim O, Barenholz Y, Fleissig O. Immune Changes Induced by Orthodontic Forces: A Critical Review. J Dent Res. 2022 Jan;101(1):11-20.
https://doi.org/10.1177/00220345211016285
PMid:34105404
Yu QY, Huang YP, Li WR. Extracellular Matrix Remodelling of the Periodontium under Orthodontic Force. Chin J Dent Res. 2024;27(2):121-31.
Behm C, Nemec M, Weissinger F, Rausch MA, Andrukhov O, Jonke E. MMPs and TIMPs Expression Levels in the Periodontal Ligament during Orthodontic Tooth Movement: A Systematic Review of In Vitro and In Vivo Studies. Int J Mol Sci. 2021 June 28;22(13):6967.
https://doi.org/10.3390/ijms22136967
PMid:34203475 PMCid:PMC8268288
Chiu KH, Karpat M, Hahn J, Chang KY, Weber M, Wolf M, et al. Cyclic Stretching Triggers Cell Orientation and Extracellular Matrix Remodeling in a Periodontal Ligament 3D In Vitro Model. Adv Healthc Mater. 2023;12(30):2301422.
https://doi.org/10.1002/adhm.202301422
PMid:37703581 PMCid:PMC11469025
Vansant L, Cadenas De LlanoPérula M, Verdonck A, Willems G. Expression of biological mediators during orthodontic tooth movement: A systematic review. Arch Oral Biol. 2018 Nov;95:170-86.
https://doi.org/10.1016/j.archoralbio.2018.08.003
PMid:30130671
Zhu Z, Sun X, Lu B, Shi Q, Tang Y, Zou S, et al. The Finite Element Analysis of Optimal Orthodontic Force for Canine Distalization with LongArm Brackets. J Biosci Med. 2025;13(01):196-205.
https://doi.org/10.4236/jbm.2025.131016
Akl HE, ElBeialy AR, ElGhafour MA, Abouelezz AM, El Sharaby FA. Root resorption associated with maxillary buccal segment intrusion using variable force magnitudes. Angle Orthod. 2021 Nov 1;91(6):733-42.
https://doi.org/10.2319/012121-62.1
PMid:34270689 PMCid:PMC8549556
Gupta S, Gupta G, Sharma M, Sharma PA, Goyal S, Kumar P. An Evaluation of the Stress Pattern Distribution for Orthodontic Tooth Movements - A Finite Element Study. Dent J Adv Stud. 2015;03:091-6.
https://doi.org/10.1055/s-0038-1672021
Moga R, Olteanu C, Delean A. Ischemic Risks Induced by Larger Orthodontic Forces on Dental Pulp and NeuroVascular Bundle in Reduced Periodontium. J Clin Med. 2024;13(22):6698.
https://doi.org/10.3390/jcm13226698
PMid:39597842 PMCid:PMC11594315
Ghaleb S, Tamish N, ElKenany W, Guindi M. The effect of two different types of forces on possible root resorption in relation to dentin phosphoprotein levels: a singleblind, splitmouth, randomized controlled trial. Prog Orthod. 2021 Dec 20;22:44.
https://doi.org/10.1186/s40510-021-00388-y
PMid:34927213 PMCid:PMC8685187
Ozkalayci N, Karadeniz E, ElekdagTurk S, Turk T, Cheng LL, Darendeliler M. Effect of continuous versus intermittent orthodontic forces on root resorption: A microcomputed tomography study. Angle Orthod. 2018;88 6:733-9.
https://doi.org/10.2319/012518-68.1
PMid:30124325 PMCid:PMC8174074
Danz JC, Degen M. Selective modulation of the bone remodeling regulatory system through orthodontic tooth movement a review. Front Oral Health [Internet]: 2025 Mar 6 [cited 2025 Aug 25]; Available from: https://www.frontiersin.org/journals/oralhealth/articles/10.3389/froh.2025.1472711/full
https://doi.org/10.3389/froh.2025.1472711
PMid:40115506 PMCid:PMC11924204
Ono T, Nakashima T. Recent advances in osteoclast biology. Histochem Cell Biol. 2018 Apr;149(4):325-41.
https://doi.org/10.1007/s00418-018-1636-2
PMid:29392395
Udagawa N, Takahashi N, Jimi E, Matsuzaki K, Tsurukai T, Itoh K, et al. Osteoblasts/stromal cells stimulate osteoclast activation through expression of osteoclast differentiation factor/RANKL but not macrophage colonystimulating factor. Bone. 1999 Nov;25(5):517-23.
https://doi.org/10.1016/S8756-3282(99)00210-0
PMid:10574571
Kumar DrIG, Raghunath DrN, H DrJ. RANKRANKLOPG: A current trends in orthodontic tooth movement and its role in accelerated orthodontics. Int J Appl Dent Sci. 2022 Apr 1;8(2):630-5.
https://doi.org/10.22271/oral.2022.v8.i2i.1568
Glass DA, Bialek P, Ahn JD, Starbuck M, Patel MS, Clevers H, et al. Canonical Wnt Signaling in Differentiated Osteoblasts Controls Osteoclast Differentiation. Dev Cell. 2005 May;8(5):751-64.
https://doi.org/10.1016/j.devcel.2005.02.017
PMid:15866165
Asano M, Yamaguchi M, Nakajima R, Fujita S, Utsunomiya T, Yamamoto H, et al. IL-8 and MCP-1 induced by excessive orthodontic force mediates odontoclastogenesis in periodontal tissues. Oral Dis. 2011 July;17(5):489-98.
https://doi.org/10.1111/j.1601-0825.2010.01780.x
PMid:21496183
Lin T, Yang L, Zheng W, Zhang B. Matrix metalloproteinases and Th17 cytokines in the gingival crevicular fluid during orthodontic tooth movement. Eur J Paediatr Dent. 2021 June;22(2):135-8.
Inchingolo F, Inchingolo AM, Malcangi G, Ferrante L, Trilli I, Di Noia A, et al. The Interaction of Cytokines in Orthodontics: A Systematic Review. Appl Sci. 2024 June 13;14(12):5133.
https://doi.org/10.3390/app14125133
Noguchi T, Kitaura H, Marahleh A, Ohori F, Nara Y, Pramusita A, et al. Tumor necrosis factorα enhances the expression of vascular endothelial growth factor in a mouse orthodontic tooth movement model. J Dent Sci. 2022 Jan;17(1):415-20.
https://doi.org/10.1016/j.jds.2021.08.011
PMid:35028065 PMCid:PMC8739756
Nguyen VT, Nardini M, Ruggiu A, Cancedda R, Descalzi F, Mastrogiacomo M. Platelet Lysate Induces in Human Osteoblasts Resumption of Cell Proliferation and Activation of Pathways Relevant for Revascularization and Regeneration of Damaged Bone. Int J Mol Sci. 2020 July 20;21(14):5123.
https://doi.org/10.3390/ijms21145123
PMid:32698534 PMCid:PMC7403959
Zhang L, Wang M, Qiu H, Wei Y, Zhou L, Nian N, et al. Epicatechin gallate promotes vascularization in coculture of human osteoblasts and outgrowth endothelial cells. Exp Biol Med. 2023 Apr;248(8):732-45.
https://doi.org/10.1177/15353702231171894
PMid:37354086 PMCid:PMC10408553
Garlet TP, Coelho U, Silva J, Garlet G. Cytokine expression pattern in compression and tension sides of the periodontal ligament during orthodontic tooth movement in humans. Eur J Oral Sci. 2007;115 5:355-62.
https://doi.org/10.1111/j.1600-0722.2007.00469.x
PMid:17850423
AvornicCiumeico L, Trifan V, Uzun I, Calfa S, Zumbreanu I, Ciumeico I. The role of the inflammatory process in orthodontic tooth movement. J Stomatol Med [Internet]: 2024 June [cited 2025 Aug 25]; Available from: https://ibn.idsi.md/sites/default/files/imag_file/3335_34.pdf
https://doi.org/10.53530/1857-1328.24.1.14
Behnaz M, Jazaeri M, Aghandeh P, Taheri M, GhafouriFard S. Genetic factors in determination of risk of external apical root resorption: A concise review. Gene Rep. 2020 Dec;21:100850.
https://doi.org/10.1016/j.genrep.2020.100850
Yamaguchi M, Fukasawa S. Is Inflammation a Friend or Foe for Orthodontic Treatment?: Inflammation in Orthodontically Induced Inflammatory Root Resorption and Accelerating Tooth Movement. Int J Mol Sci. 2021 Feb 27;22(5):2388.
https://doi.org/10.3390/ijms22052388
PMid:33673606 PMCid:PMC7957544
CastilloMontaño L, ColinoGallardo P, BaptistaSanchez H, Drewling I, AlvaradoLorenzo M, AntonioZancajo L, et al. Efficacy of Invasive and NonInvasive Methods in Orthodontic Tooth Movement Acceleration: A Systematic Review. Appl Sci. 2024 Nov 19;14(22):10700.
https://doi.org/10.3390/app142210700
Fleming PS, Andrews J. Periodontitis: orthodontic implications and management. Br Dent J. 2024 Sept 13;237(5):334-40.
https://doi.org/10.1038/s41415-024-7789-6
PMid:39271869 PMCid:PMC11399084
Ristoska S, Dzipunova B, Stefanovska E, Rendzova V, RadojkovaNikolovska V, Evrosimovska B. Orthodontic Treatment of a Periodontally Affected Adult Patient (Case Report). Open Access Maced J Med Sci. 2019 July 20;7(14):2343-9.
https://doi.org/10.3889/oamjms.2019.629
PMid:31592049 PMCid:PMC6765088
Papageorgiou SN, Papadelli AA, Eliades T. Effect of orthodontic treatment on periodontal clinical attachment: a systematic review and metaanalysis. Eur J Orthod. 2018 Apr 6;40(2):176-94.
https://doi.org/10.1093/ejo/cjx052
PMid:29106513
Jepsen K, Sculean A, Jepsen S. Complications and treatment errors involving periodontal tissues related to orthodontic therapy. Periodontol 2000. 2023 June;92(1):135-58.
https://doi.org/10.1111/prd.12484
PMid:36920050
Peterson BW, Tjakkes G, Renkema A, Manton DJ, Ren Y. The oral microbiota and periodontal health in orthodontic patients. Periodontol 2000. 2024;00:1-19.
https://doi.org/10.1111/prd.12594
PMid:39031969
Zargham A, Geramy A, Rouhi G. Evaluation of longterm orthodontic tooth movement considering bone remodeling process and in the presence of alveolar bone loss using finite element method. Orthod Waves. 2016 Dec 1;75(4):85-96.
https://doi.org/10.1016/j.odw.2016.09.001
Almutairi RM, Alturaif DJ, Alanzi LM. Importance of Oral Hygiene in Orthodontic Treatment. Saudi J Oral Dent Res. 2023 Mar 3;8(03):100-9.
https://doi.org/10.36348/sjodr.2023.v08i03.001
Shumynska T, Melnichuk T. Longterm results of treatment of periodontal diseases in children in the dynamics of orthodontic treatment with fixed appliances. Suchasna Stomatol. 2025;124(1):349.
https://doi.org/10.33295/1992-576X-2025-1-34
Akbar A, Chheena A, Mansoor S, Zulfiqar RMF, Saeed F, Butt H. Effect of Periodontal Scaling in Patients Undergoing Orthodontic Treatment on General Oral and Periodontal Health. J Health Rehabil Res. 2024 May 15;4(2):754-8.
https://doi.org/10.61919/jhrr.v4i2.939
Erbe C, Heger S, Kasaj A, Berres M, Wehrbein H. Orthodontic treatment in periodontally compromised patients: a systematic review. Clin Oral Investig. 2022 Dec 11;27(1):79-89.
https://doi.org/10.1007/s00784-022-04822-1
PMid:36502508 PMCid:PMC9877066
Gehlot M, Sharma R, Tewari S, Kumar D, Gupta A. Effect of orthodontic treatment on periodontal health of periodontally compromised patients. Angle Orthod. 2022 May 1;92(3):324-32.
https://doi.org/10.2319/022521-156.1
PMid:34882193 PMCid:PMC9020398
Krausz E, Einy S, Aizenbud D, Levin L. Orthodontic treatment in periodontal patients. Refuat HaPeh VehaShinayim. 2011;28 3:38-49, 70.
Tietmann C, Bröseler F, Axelrad T, Jepsen K, Jepsen S. Regenerative periodontal surgery and orthodontic tooth movement in stage IV periodontitis: A retrospective practice-based cohort study. J Clin Periodontol. 2021 May;48(5):668-78.
https://doi.org/10.1111/jcpe.13442
PMid:33555608
Jepsen K, Tietmann C, Kutschera E, Wüllenweber P, Jäger A, Cardaropoli D, et al. The effect of timing of orthodontic therapy on the outcomes of regenerative periodontal surgery in patients with stage IV periodontitis: A multicenter randomized trial. J Clin Periodontol. 2021 Oct;48(10):1282-92.
https://doi.org/10.1111/jcpe.13528
PMid:34312872
Tu CC, Lo CY, Chang PC, Yin HJ. Orthodontic treatment of periodontally compromised teeth after periodontal regeneration: A restrospective study. J Formos Med Assoc. 2022 Oct;121(10):2065-73.
https://doi.org/10.1016/j.jfma.2022.02.021
PMid:35305894
Deandra FA, Sulijaya B, Sudjatmika DA, Harsas NA. Selection of bone graft material and proper timing of periodontal surgery for orthodontic patients: A systematic review. Heliyon. 2024 Jan 15;10(1):e24201.
https://doi.org/10.1016/j.heliyon.2024.e24201
PMid:38268591 PMCid:PMC10806355
Miao Y, Chang YC, Tanna N, Almer N, Chung CH, Zou M, et al. Impact of Frontier Development of Alveolar Bone Grafting on Orthodontic Tooth Movement. Front Bioeng Biotechnol. 2022 June 30;10:869191.
https://doi.org/10.3389/fbioe.2022.869191
PMid:35845390 PMCid:PMC9280714
Martin C, Sanz M. Orthodontic tooth movement after periodontal regeneration of intrabony defects. Korean J Orthod. 2024 Jan 25;54(1):3-15.
https://doi.org/10.4041/kjod24.007
PMid:38268459 PMCid:PMC10811355
Ghezzi C, Viganò VM, Francinetti P, Zanotti G, Masiero S. Orthodontic Treatment After Induced Periodontal Regeneration in Deep Infrabony Defects. Clin Adv Periodontics. 2013 Feb;3(1):24-31.
https://doi.org/10.1902/cap.2012.110085
Ashfaq R, Kovács A, Berkó S, BudaiSzűcs M. Developments in Alloplastic Bone Grafts and Barrier Membrane Biomaterials for Periodontal Guided Tissue and Bone Regeneration Therapy. Int J Mol Sci. 2024 July 15;25(14):7746.
https://doi.org/10.3390/ijms25147746
PMid:39062989 PMCid:PMC11277074
Xiang C, Zhang L, Tao E. Research progress of enamel matrix derivative on periodontal tissue regeneration: a narrative review. Front Dent Med. 2025 June 30;6:1611402.
https://doi.org/10.3389/fdmed.2025.1611402
PMid:40661224 PMCid:PMC12256556
Ogihara S, Wang H. Periodontal Regeneration With or Without Limited Orthodontics for the Treatment of 2- or 3-Wall Infrabony Defects. J Periodontol. 2010 Dec;81(12):1734-42.
https://doi.org/10.1902/jop.2010.100127
PMid:20629545
Tietmann C, Jepsen S, Heibrok H, Wenzel S, Jepsen K. Long-term stability of regenerative periodontal surgery and orthodontic tooth movement in stage IV periodontitis: 10-year data of a retrospective study. J Periodontol. 2023 Oct;94(10):1176-86.
https://doi.org/10.1002/JPER.23-0081
PMid:37010261
Ardila CM, Pertuz M, VivaresBuiles AM. Clinical Efficacy of Platelet Derivatives in Periodontal Tissue Regeneration: An Umbrella Review Casarin R, editor. Int J Dent. 2023 July 3;2023:1-15.
https://doi.org/10.1155/2023/1099013
PMid:37435111 PMCid:PMC10332916
Feu D. Orthodontic treatment of periodontal patients: challenges and solutions, from planning to retention. Dent Press J Orthod. 2020 Dec;25(6):79-116.
https://doi.org/10.1590/2177-6709.25.6.079-116.sar
PMid:33503129 PMCid:PMC7869805
Isler AAA. Orthodontıc treatment and oral flora. Asian J Med Biol Res. 2022 Nov 4;8(4):181-6.
https://doi.org/10.3329/ajmbr.v8i4.62167
Roberts HM, Yonel Z, Kantarci A, Grant MM, Chapple IL. Impact of gingivitis on circulating neutrophil reactivity and gingival crevicular fluid inflammatory proteins. Int J Environ Res Public Health. 2022;19(10):6339.
https://doi.org/10.3390/ijerph19106339
PMid:35627876 PMCid:PMC9141451
Chatzisymeonidou S, Papadopoulos P, Andreadis D, Poulopoulos A. Desquamative gingivitis: Clinical and epidemiological findings in patients from Northern Greece. Balk J Dent Med. 2023;27(3):148-53.
https://doi.org/10.5937/bjdm2303148C
Sum FHKMH, Shan Z, Chan YHD, Chu RJDH, Pelekos G, She TT. Biomechanical Considerations in the Orthodontic Treatment of a Patient with Stabilised Stage IV Grade C Generalised Periodontitis: A Case Report. Bioengineering. 2024 Apr 19;11(4):403.
https://doi.org/10.3390/bioengineering11040403
PMid:38671824 PMCid:PMC11048569
Zhang Y, Yan J, Zhang Y, Liu H, Han B, Li W. Agerelated alveolar bone maladaptation in adult orthodontics: finding new ways out. Int J Oral Sci. 2024 Aug 1;16(1):52.
https://doi.org/10.1038/s41368-024-00319-7
PMid:39085217 PMCid:PMC11291511
Ugarte OM, Cattaneo PM, Roscoe MG, Onone IG, Dominguez GC, Meira JBC. Optimal Intrusive Force for a Periodontally Compromised Tooth: A Finite Element Analysis Strategy. Dent Mater. 2022;38:e28-9.
https://doi.org/10.1016/j.dental.2021.12.076
Sabbagh H, Haas E, Baumert U, Seidel CL, Hötzel L, Wichelhaus A. Biomechanical Simulation of Orthodontic EnBloc Retraction Comparing Compound Technique and Sliding Mechanics Using a HOSEA Robotic Device. Bioengineering. 2024 Feb 2;11(2):153.
https://doi.org/10.3390/bioengineering11020153
PMid:38391639 PMCid:PMC10886252
Kalina E, Machoy M, Górski B. Interdisciplinary Approaches by Polish Orthodontists, Periodontists, and Oral Surgeons to Soft Tissue Augmentation in Adult Patients: A Survey Study. Appl Sci. 2024 Oct 22;14(21):9647.
https://doi.org/10.3390/app14219647
Rashid ZJ, Gul SS, Shaikh MS, Abdulkareem AA, Zafar MS. Incidence of Gingival Black Triangles following Treatment with Fixed Orthodontic Appliance: A Systematic Review. Healthcare. 2022 July 24;10(8):1373.
https://doi.org/10.3390/healthcare10081373
PMid:35893195 PMCid:PMC9331869
Jung JS, Lim HK, Lee YS, Jung SK. The Occurrence and Risk Factors of Black Triangles Between Central Incisors After Orthodontic Treatment. Diagnostics. 2024 Jan;14(23):2747.
https://doi.org/10.3390/diagnostics14232747
PMid:39682655 PMCid:PMC11640695
Patel M, Guni A, Nibali L, GarciaSanchez R. Interdental papilla reconstruction: a systematic review. Clin Oral Investig. 2024 Jan 17;28(1):101.
https://doi.org/10.1007/s00784-023-05409-0
PMid:38231354 PMCid:PMC10794407
Dong J chen, Liao Y, Sun M jun, Gong Y, Chen H wen, Song Z chen. Modified interproximal tunneling technique with customized subepithelial connective tissue graft for gingival papilla reconstruction: report of three cases with a cutback incision on the palatal side. BMC Oral Health. 2023 Oct 26;23(1):800.
https://doi.org/10.1186/s12903-023-03525-7
PMid:37884939 PMCid:PMC10605313
Hashim NT, Dasnadi SP, Ziada H, Rahman MM, Ahmed A, Mohammed R, et al. Orthodontic Management of Different Stages and Grades of Periodontitis According to the 2017 Classification of Periodontal Diseases. Dent J. 2025 Feb;13(2):59.
https://doi.org/10.3390/dj13020059
PMid:39996933 PMCid:PMC11853809
Yan T, Li H, Yan J, Ma S, Tan J. Age-related mitophagy regulates orthodontic tooth movement by affecting PDLSCs mitochondrial function and RANKL/OPG. FASEB J. 2024 Aug 15;38(15):e23865.
https://doi.org/10.1096/fj.202401280R
PMid:39096136
Kim H, Jo H, Cha JY, Lee KJ, Yu HS, Choi SH. Orthodontic treatment of a middleaged patient with periodontally compromised dentition accompanied by pathologic tooth migration. Angle Orthod. 2024 Nov;94(6):678-86.
https://doi.org/10.2319/122923-866.1
PMid:39194956 PMCid:PMC11493424
Salvesen BF, Grytten J, Rongen G, VandevskaRadunovic V. PatientReported Outcome Measures on Oral Hygiene, Periodontal Health, and Treatment Satisfaction of Orthodontic Retention Patients up to Ten Years after Treatment A CrossSectional Study. Int J Environ Res Public Health. 2022 Apr 15;19(8):4843.
https://doi.org/10.3390/ijerph19084843
PMid:35457707 PMCid:PMC9027940
Almasri AMH, Hajeer MY, Ajaj MA, Almusawi AOA, Jaber ST, Zakaria AS, et al. Patient Satisfaction Following Orthodontic Treatment A Systematic Review. Cureus [Internet]: 2024 July 25 [cited 2025 Sept 4]; Available from: https://www.cureus.com/ articles/278470-patient-satisfaction-following-orthodontic-treatment-a-systematic-review
https://doi.org/10.7759/cureus.65339
Dipalma G, Inchingolo AD, Fiore A, Balestriere L, Nardelli P, Casamassima L, et al. The Differential Impact of Clear Aligners and Fixed Orthodontic Appliances on Periodontal Health: A Systematic Review. Children. 2025 Jan 26;12(2):138.
https://doi.org/10.3390/children12020138
PMid:40003240 PMCid:PMC11854263
Zhao J, Feng Z, Liu Y, Sun S, Feng Z. Advances in orthodontic treatment for periodontal disease: a bibliometric analysis, emerging insights and clinical implications. Front Dent Med. 2025;6:1600672.
https://doi.org/10.3389/fdmed.2025.1600672
PMid:40777165 PMCid:PMC12328451
articles/278470patientsatisfactionfollowingorthodontictreatmentasystematicreview
Dipalma G, Inchingolo AD, Fiore A, Balestriere L, Nardelli P, Casamassima L, et al. The Differential Impact of Clear Aligners and Fixed Orthodontic Appliances on Periodontal Health: A Systematic Review. Children. 2025 Jan 26;12(2):138.
https://doi.org/10.3390/children12020138
PMid:40003240 PMCid:PMC11854263
Zhao J, Feng Z, Liu Y, Sun S, Feng Z. Advances in orthodontic treatment for periodontal disease: a bibliometric analysis, emerging insights and clinical implications. Front Dent Med. 2025;6:1600672.
https://doi.org/10.3389/fdmed.2025.1600672
PMid:40777165 PMCid:PMC12328451
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Galen Medical Journal

This work is licensed under a Creative Commons Attribution 4.0 International License.







