Gentamicin-Loaded Chitosan Nanoparticles Improve Its Therapeutic Effects on Brucella-Infected J774A.1 Murine Cells
DOI:
https://doi.org/10.31661/gmj.v8i.1296Keywords:
Brucella melitennis, Brucella abortus, Chitosan, Gentamicin, NanoparticlesAbstract
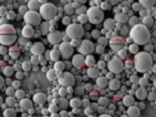
Background: Final elimination of some intracellular bacterial agents, such as Brucella, is often a complex issue and impossible to achieve, primarily due to the presence and survival of the bacteria within phagocytic cells. By penetrating into the cell membrane, drug delivery nanosystems can reduce the number of intracellular bacteria. The aim of this study was to assess the efficacy of chitosan nanoparticles on the delivery of gentamicin into Brucella infected J774A.1 murine cells in vitro. Materials and Methods: Chitosan nanoparticles (NPs) were synthesized using ionic gelation technique. The shape, size and charge of NPs, loading rate and release of the drug were investigated. Finally, the effects of gentamicin-loaded chitosan NPs (Gen-Cs) and free gentamicin on J774A.1 murine cells infected with these bacteria were examined. Results: The mean size and charge of NPs were computed as 100 nm and +28mV, respectively. The loading capacity of NPs was 22%. About 70% of the drug was released from NPs during the first 8 hours. Antimicrobial activity of the two formulations showed that MIC (minimum inhibitory concentration) of the Gen-Cs and free drug was 3.1 and 6.25 µg, respectively. The minimum bactericidal concentration of the NPs-loaded drug and free drug was 6.25 and 12.5 µg, respectively. Cell culture analysis revealed that there was a significant reduction in the load of the intercellular bacteria in J774A.1 murine cells in both formulations. Conclusion: Our results showed the Gen-Cs have a proper potential for optimal treatment of intracellular bacterial agents. [GMJ.2019;8:e1296]Â
References
Jennings GJ, Hajjeh RA, Girgis FY, Fadeel MA, Maksoud MA, Wasfy MO, et al. Brucellosis as a cause of acute febrile illness in Egypt. Trans R Soc Trop Med Hyg. 2007;101(7):707-13. https://doi.org/10.1016/j.trstmh.2007.02.027PMid:17442354 Seleem MN, Boyle SM, Sriranganathan N. Brucella: a pathogen without classic virulence genes. Vet. Microbiol. 2008;129(1):1-14. https://doi.org/10.1016/j.vetmic.2007.11.023PMid:18226477 Rolain J-M, Maurin M, Raoult D. Bactericidal effect of antibiotics on Bartonella and Brucella spp. clinical implications. J Antimicrob Chemother. 2000;46(5):811-4. https://doi.org/10.1093/jac/46.5.811PMid:11062204 Acocella G, Bertrand A, Beytout J, Durrande JB, Rodriguez J-AG, Kosmidis J, et al. Comparison of three different regimens in the treatment of acute brucellosis: a multicenter multinational study. J Antimicrob Chemother. 1989;23(3):433-9. https://doi.org/10.1093/jac/23.3.433PMid:2732125 Ariza J, Bosilkovski M, Cascio A, Colmenero JD, Corbel MJ, Falagas ME, et al. Perspectives for the treatment of brucellosis in the 21st century: the Ioannina recommendations. PLoS Med. 2007;4(12):e317. https://doi.org/10.1371/journal.pmed.0040317PMid:18162038 PMCid:PMC2222927 Ersoy Y, Sonmez E, Tevfik MR, But AD. Comparison of three different combination therapies in the treatment of human brucellosis.Med Sante Trop. 2005;35(4):210-2. https://doi.org/10.1258/004947505774938765PMid:16354469 Brucellosis JFWECo. Joint FAO/WHO Expert Committee on Brucellosis: Sixth Report: World Health Organization; 1986. Zembower TR, Noskin GA, Postelnick MJ, Nguyen C, Peterson LR. The utility of aminoglycosides in an era of emerging drug resistance. Int J Antimicrob Agents. 1998;10(2):95-105. https://doi.org/10.1016/S0924-8579(98)00033-8 Solera J, Martinez-Alfaro E, Espinosa A. Recognition and optimum treatment of brucellosis. Drugs. 1997;53(2):245-56. https://doi.org/10.2165/00003495-199753020-00005PMid:9028744 Taber HW, Mueller J, Miller P, Arrow A. Bacterial uptake of aminoglycoside antibiotics. Microbiol Mol Biol Rev. 1987;51(4):439. Tulkens PM. Intracellular pharmacokinetics and localization of antibiotics as predictors of their efficacy against intraphagocytic infections. Scand J .Infect Dis Suppl. 1990;74:209-17. Dutt M, Khuller G. Chemotherapy of Mycobacterium tuberculosis infections in mice with a combination of isoniazid and rifampicin entrapped in Poly (DL-lactide-co-glycolide) microparticles. J Antimicrob Chemother. 2001;47(6):829-35. https://doi.org/10.1093/jac/47.6.829PMid:11389115 Quenelle DC, Staas JK, Winchester GA, Barrow EL, Barrow WW. Efficacy of Microencapsulated Rifampin in Mycobacterium tuberculosis-Infected Mice. Antimicrob Agents Chemother. 1999;43(5):1144-51. https://doi.org/10.1128/AAC.43.5.1144PMid:10223927 PMCid:PMC89124 Schiffelers R, Storm G, Bakker-Woudenberg I. Liposome-encapsulated aminoglycosides in pre-clinical and clinical studies. J Antimicrob Chemother. 2001;48(3):333-44. https://doi.org/10.1093/jac/48.3.333PMid:11532996 Swenson CE, Stewart K, Hammett J, Fitzsimmons W, Ginsberg R. Pharmacokinetics and in vivo activity of liposome-encapsulated gentamicin. Antimicrob Agents Chemother1990;34(2):235-40. https://doi.org/10.1128/AAC.34.2.235PMid:2183715 PMCid:PMC171564 Armstead AL, Li B. Nanomedicine as an emerging approach against intracellular pathogens. Int J Nanomedicine. 2011;6:3281. https://doi.org/10.2147/IJN.S27285PMid:22228996 PMCid:PMC3252676 Imbuluzqueta E, Gamazo C, Ariza J, Blanco-Prieto MJ. Drug delivery systems for potential treatment of intracellular bacterial infections. Front. Biosci. 2010. https://doi.org/10.2741/3627PMid:20036827 Lecaroz MC, Blanco-Prieto MJ, Campanero MA, Salman H, Gamazo C. Poly (D, L-lactide-coglycolide) particles containing gentamicin: pharmacokinetics and pharmacodynamics in Brucella melitensis-infected mice. Antimicrob Agents Chemother. 2007;51(4):1185-90. https://doi.org/10.1128/AAC.00809-06PMid:17220415 PMCid:PMC1855454 Prior S, Gander B, Irache JM, Gamazo C. Gentamicin-loaded microspheres for treatment of experimental Brucella abortus infection in mice. J Antimicrob Chemother. 2005;55(6):1032-6. https://doi.org/10.1093/jac/dki144PMid:15883176 Govender T, Riley T, Ehtezazi T, Garnett MC, Stolnik S, Illum L, et al. Defining the drug incorporation properties of PLA-PEG nanoparticles. Int J Pharm. 2000;199(1):95-110. https://doi.org/10.1016/S0378-5173(00)00375-6 Atyabi F, Moghaddam FA, Dinarvand R, Zohuriaan-Mehr MJ, Ponchel G. Thiolated chitosan coated poly hydroxyethyl methacrylate nanoparticles: synthesis and characterization. Carbohydr Polym. 2008;74(1):59-67. https://doi.org/10.1016/j.carbpol.2008.01.015 Calvo P, Vila-Jato JL, Alonso MaJ. Evaluation of cationic polymer-coated nanocapsules as ocular drug carriers. Int J Pharm. 1997;153(1):41-50. https://doi.org/10.1016/S0378-5173(97)00083-5 Ji J, Hao S, Wu D, Huang R, Xu Yct it. Preparation, characterization and in vitro release of chitosan nanoparticles loaded with gentamicin and salicylic acid. Carbohydr Polym. 2011;85(4):803-8. https://doi.org/10.1016/j.carbpol.2011.03.051 Anal AK, Stevens WF, Remunan-Lopez C. Ionotropic cross-linked chitosan microspheres for controlled release of ampicillin. Int J Pharm. 2006;312(1-2):166-73. https://doi.org/10.1016/j.ijpharm.2006.01.043PMid:16497452 Kaminski HM, Feix JB. Effects of D-lysine substitutions on the activity and selectivity of antimicrobial peptide CM15. Polymers. 2011;3(4):2088-106. https://doi.org/10.3390/polym3042088PMid:30405905 PMCid:PMC6217857 Lee Y-S, Jang K, Cha J-D. Synergistic antibacterial effect between silibinin and antibiotics in oral bacteria.Biomed Res Int. 2011;2012.27. https://doi.org/10.1155/2012/618081PMid:21941436 PMCid:PMC3173953 Chuah LH, Roberts CJ, Billa N, Abdullah S, Rosli R. Cellular uptake and anticancer effects of mucoadhesive curcumin-containing chitosan nanoparticles. Colloids Surf B Biointerfaces. 2014;116:228-36. https://doi.org/10.1016/j.colsurfb.2014.01.007PMid:24486834 Garaiova Z, Strand SP, Reitan NK, Lélu S, Størset SØ, Berg K, et al. Cellular uptake of DNA-chitosan nanoparticles: The role of clathrin-and caveolae-mediated pathways. Int J Biol Macromol. 2012;51(5):1043-51. https://doi.org/10.1016/j.ijbiomac.2012.08.016PMid:22947453 Salatin S, Maleki Dizaj S, Yari Khosroushahi A. Effect of the surface modification, size, and shape on cellular uptake of nanoparticles. Int J Biochem Cell Biol. 2015;39(8):881-90. https://doi.org/10.1002/cbin.10459PMid:25790433 Drevets DA, Canono BP, Leenen P, Campbell PA. Gentamicin kills intracellular Listeria monocytogenes.Infect Immun. 1994;62(6):2222-8. Prior S, Gander B, Lecároz C, Irache JM, Gamazo C. Gentamicin-loaded microspheres for reducing the intracellular Brucella abortus load in infected monocytes. J Antimicrob Chemother. 2004;53(6):981-8. https://doi.org/10.1093/jac/dkh227PMid:15102748 Imbuluzqueta E, Gamazo C, Lana H, Campanero MÃ, Salas D, Gil AG, et al. Hydrophobic gentamicin-loaded nanoparticles are effective against Brucella melitensis infection in mice. Antimicrob Agents Chemother. 2013;57(7):3326-33. https://doi.org/10.1128/AAC.00378-13PMid:23650167 PMCid:PMC3697350